Introduction
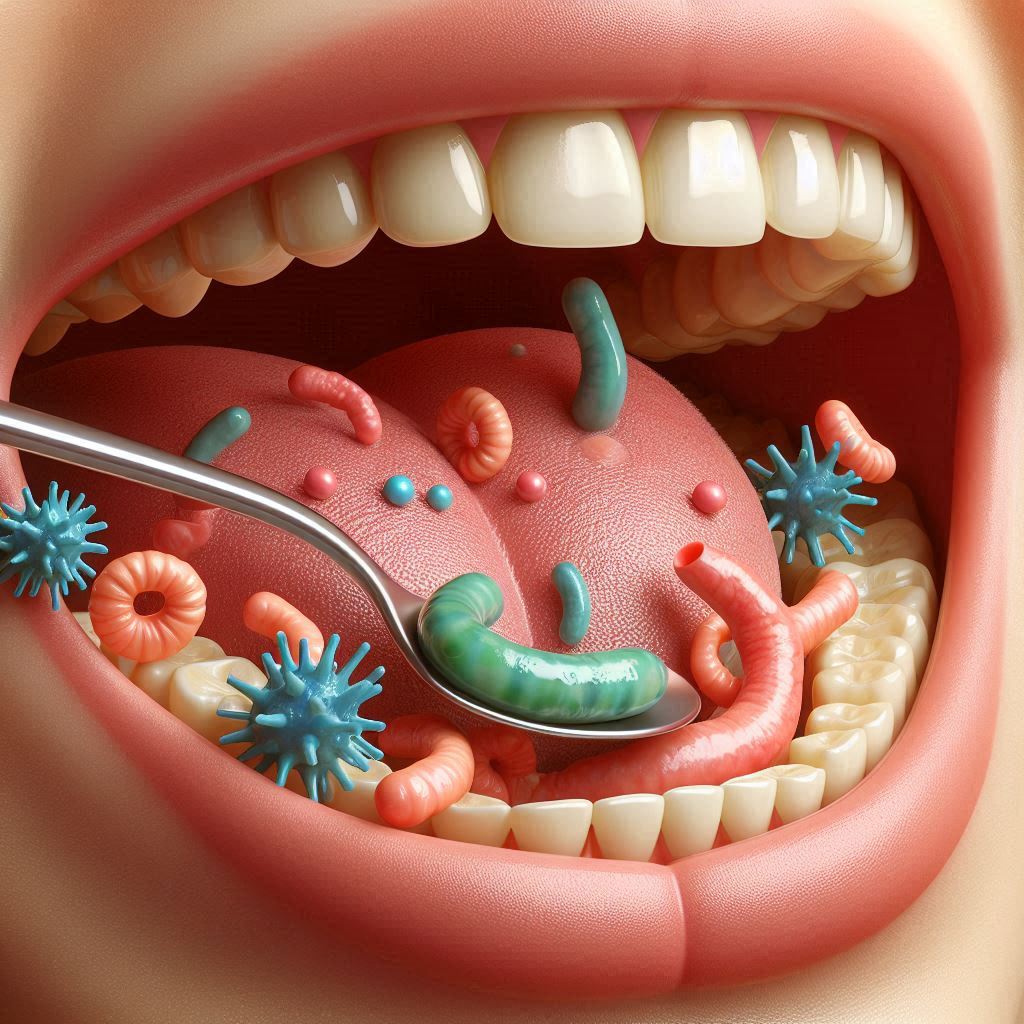
The human body is host to a vast and intricate network of microorganisms, comprising trillions of bacteria, fungi, viruses, and other microbes. These microorganisms collectively form what is called the microbiome, and they are critical to a multitude of bodily functions, ranging from digestion and immune regulation to mental health and disease prevention. While most people are familiar with the fact that the microbiome in our gut plays an essential role in digestion, fewer may be aware of the interconnectedness between the gut and other bodily systems, including the mouth. Recent research suggests that there is a complex and important relationship between stomach bacteria and oral health, and disturbances in the gut microbiome may contribute significantly to issues such as gum disease, tooth decay, and bad breath. This guide will explore how bacteria in the stomach may be affecting your oral health, with a detailed focus on the biological mechanisms, gut-mouth axis, and practical advice to manage this connection.
Understanding the Microbiome: An Overview
The human microbiome consists of trillions of microbes that live in and on the body. These microbes are involved in digestion, immunity, metabolism, and many other processes. The largest concentration of bacteria is found in the intestines, particularly the large intestine, where they assist in breaking down food and absorbing nutrients. In addition to the gut, other areas of the body have their own microbiomes, including the skin, lungs, and mouth.
The oral microbiome refers to the community of microorganisms that inhabit the mouth. This includes bacteria that help break down food particles and maintain the health of the mouth’s tissues, as well as potential pathogenic bacteria that can cause disease. Similarly, the stomach and intestines have their own microbiota, with unique bacterial populations that thrive in highly acidic environments. While these microbiomes are distinct, they are interconnected. The state of one can influence the others, as they communicate through various biological pathways, including immune system interactions, inflammatory responses, and even bacterial migration. Dysbiosis, or an imbalance of the microbial communities in any of these areas, can lead to various health issues.
The Gut and Mouth Connection: How Stomach Bacteria Affect Oral Health
The Inflammatory Pathway: How Gut Inflammation Can Affect Oral Health
One of the primary ways that stomach bacteria can influence oral health is through the inflammatory pathways that extend from the gut. Chronic gut inflammation—often resulting from conditions such as irritable bowel syndrome (IBS), Crohn’s disease, or gastric ulcers—can lead to systemic inflammation throughout the body. This is not limited to the digestive tract but can affect other tissues, including those in the oral cavity.
Gastritis and Periodontitis
Gastritis, which is inflammation of the stomach lining, is often caused by an overgrowth of harmful bacteria such as Helicobacter pylori. This bacterium is also linked to peptic ulcers and has been shown to contribute to inflammation in the stomach. Interestingly, studies have also suggested a potential link between H. pylori and periodontitis, a severe form of gum disease that can result in tooth loss if left untreated. In patients with chronic H. pylori infections, there appears to be an elevated level of systemic inflammation, which could, in turn, exacerbate gum inflammation and promote the progression of periodontal disease.
Similarly, the overgrowth of other harmful bacteria in the stomach, such as those involved in irritable bowel syndrome or other gut disorders, can promote a state of chronic low-grade inflammation. This systemic inflammation can travel to the oral tissues, impairing gum health, weakening the immune response in the mouth, and making the gums more susceptible to infections and diseases.
Immune System Interactions: How the Gut-Mouth Axis Impacts Oral Defenses
The gut and the mouth are connected through the immune system. Both the gut and oral cavities contain a network of immune cells, including T-cells, macrophages, and antibodies, which serve to protect the body from pathogens. Disruptions in the gut microbiome can affect the body’s immune response, leading to heightened vulnerability to infections, including those in the mouth.
Gut Dysbiosis and Immune Modulation
When the balance of bacteria in the gut is disrupted—a condition known as gut dysbiosis—the immune system can become overstimulated. This overstimulation leads to an imbalance in immune responses that may result in autoimmune conditions or excessive inflammatory responses. One of the key immune system components that connects the gut and mouth is immunoglobulin A (IgA), an antibody that plays a central role in mucosal immunity in both the gut and oral cavity.
IgA helps prevent the colonization of harmful bacteria by binding to them and neutralizing their effects. Dysbiosis in the gut can affect the production and function of IgA, weakening the body’s defenses against pathogens that may be present in the mouth. This makes it easier for bacteria to establish themselves in the oral cavity and cause conditions like gingivitis, periodontitis, and tooth decay.
Bacterial Migration: The Movement of Pathogens Between the Gut and Mouth
The human body is a dynamic system, and bacteria are constantly moving between different areas of the body. This includes the migration of harmful bacteria from the stomach and intestines into the oral cavity. This process can occur through several mechanisms, including swallowing bacteria-laden saliva, gastroesophageal reflux disease (GERD), and the regurgitation of stomach contents into the mouth.
Gastroesophageal Reflux Disease (GERD) and Oral Health
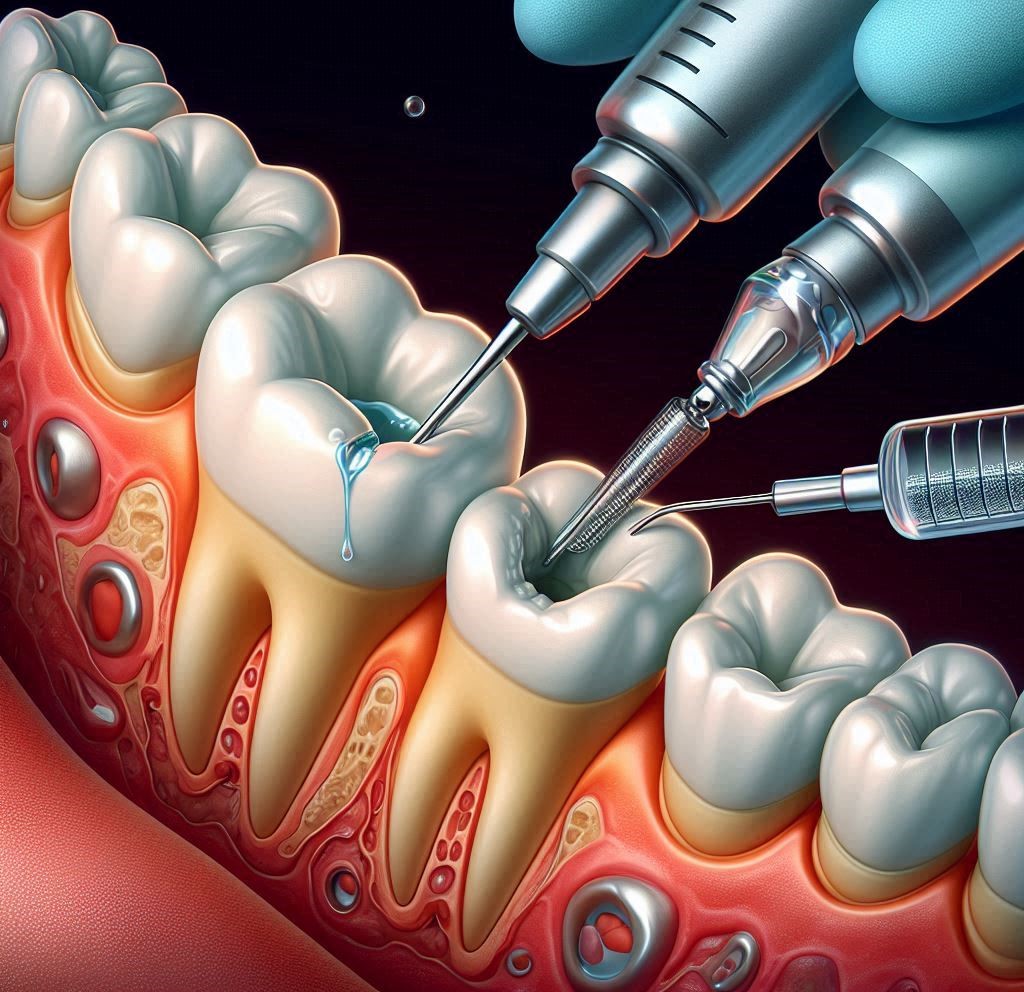
GERD is a common condition in which stomach acid, along with digestive enzymes and bacteria, is regurgitated into the esophagus and sometimes into the mouth. When this happens, the stomach’s acidic contents can erode tooth enamel, leading to increased tooth sensitivity and a higher risk of cavities. In addition, the presence of stomach bacteria in the mouth can contribute to the overgrowth of harmful bacteria, leading to issues like gum disease and bad breath.
A study of individuals with GERD found that they had a significantly higher prevalence of oral health issues, such as tooth erosion and gum disease, compared to individuals without GERD. This is partly because the acidic environment in the mouth, combined with the introduction of harmful bacteria from the stomach, creates an ideal setting for the growth of pathogenic oral bacteria.
Acidic Conditions and Tooth Erosion: The Effect of Stomach Acid on Oral Health
The stomach is an acidic environment, with a pH ranging from 1.5 to 3.5, which helps break down food and kill harmful pathogens. When stomach acid is regurgitated into the mouth, it can cause tooth enamel to erode, which is a major risk factor for tooth decay. Acidic conditions also promote the growth of acidophilic bacteria—bacteria that thrive in low pH environments—such as Streptococcus mutans, which is one of the primary culprits behind tooth decay.
The Role of Streptococcus mutans in Gut-Mouth Communication
Streptococcus mutans is a bacterium commonly associated with tooth decay and the formation of cavities. Interestingly, this bacterium can also be found in the intestines, particularly in the small intestine, and its overgrowth in the gut can contribute to oral health problems. In the mouth, S. mutans produces lactic acid by fermenting sugars, which lowers the pH and accelerates enamel erosion.
Research has shown that individuals with an overgrowth of S. mutans in the gut are more likely to have it present in their mouths as well, which can lead to a greater risk of tooth decay. Therefore, the migration of bacteria between the gut and the mouth may have a synergistic effect, amplifying the risk of both gut and oral health issues.
The Impact of Specific Stomach Bacteria on Oral Health
Not all bacteria in the stomach have the same impact on oral health, but certain bacterial species are more likely to contribute to oral health problems. Below is a detailed look at some of the key bacteria involved in the gut-mouth connection.
Helicobacter pylori and Oral Health
Helicobacter pylori is a Gram-negative bacterium that infects the stomach lining and is responsible for a variety of gastrointestinal disorders, including chronic gastritis and peptic ulcers. Recent studies have found evidence that H. pylori can be present in dental plaque, saliva, and even periodontal pockets. There is ongoing research into whether H. pylori contributes to oral health issues, such as gum disease and even oral cancer.
The presence of H. pylori in the mouth has been shown to coincide with higher levels of oral inflammation, especially in individuals with existing periodontal disease. This suggests that the bacterium may not only contribute to stomach problems but also play a role in exacerbating oral health issues.
Streptococcus mutans
While Streptococcus mutans is typically associated with dental cavities and tooth decay, it is also a common inhabitant of the digestive tract. When this bacterium overgrows in the stomach or intestines, it may contribute to the development of oral health problems, especially when it migrates to the mouth. S. mutans produces acids as part of its metabolic process, and these acids can erode tooth enamel and lead to cavities.
Lactobacillus species
Lactobacilli are beneficial bacteria that are commonly found in both the stomach and the mouth. These bacteria are known to help regulate the pH balance in the gut and the oral cavity, preventing the growth of harmful bacteria. However, an overgrowth of lactobacilli, especially in individuals with dysbiosis or an imbalanced microbiome, can lead to oral health problems such as tooth decay and gum inflammation.
Preventive Measures for Oral Health Linked to Gut Bacteria
Given the clear connection between the gut microbiome and oral health, it is crucial to adopt strategies that support both systems simultaneously. Here are several practical steps to maintain a healthy gut and mouth:
Diet and Nutrition: Feeding Your Microbiome
Maintaining a balanced diet rich in fiber, fruits, vegetables, and fermented foods is crucial for gut health. Foods like yogurt, kefir, and kimchi can introduce beneficial probiotics into the gut, while prebiotic-rich foods like garlic, onions, and leeks provide nourishment for healthy gut bacteria.
In addition, reducing your intake of sugary, highly processed foods is important for both gut and oral health, as sugar feeds harmful bacteria in both areas.
Probiotics for Gut and Oral Health
Probiotics, which are beneficial bacteria, have been shown to have positive effects on both gut and oral health. Regularly consuming probiotic-rich foods or supplements can help maintain a balanced microbiome, preventing dysbiosis and the migration of harmful bacteria into the mouth.
Oral Hygiene Practices
The cornerstone of maintaining good oral health is consistent oral hygiene. Brushing your teeth at least twice a day with fluoride toothpaste, flossing daily, and using an antibacterial mouthwash can help prevent the buildup of harmful bacteria in the mouth. Regular dental visits for professional cleanings are also essential.
Managing Acid Reflux and GERD
For individuals suffering from GERD or acid reflux, it is important to take steps to manage the condition to prevent stomach acid from reaching the mouth. This can involve dietary changes, such as avoiding acidic and fatty foods, as well as lifestyle modifications like not lying down immediately after meals and elevating the head of the bed while sleeping.
Hydration
Staying hydrated helps promote healthy saliva production, which plays a crucial role in neutralizing acids and flushing away harmful bacteria in the mouth. Drinking plenty of water throughout the day can help protect your teeth from erosion and decay.
Conclusion
The connection between stomach bacteria and oral health is a fascinating and intricate area of research that highlights the importance of maintaining a healthy, balanced microbiome throughout the body. Dysbiosis in the gut can contribute to a range of oral health issues, from gum disease and tooth decay to chronic bad breath. By adopting a holistic approach to health—focusing on proper diet, oral hygiene, and managing gut health—you can reduce the risk of these issues and support both your gut and mouth. As research into the gut-mouth connection continues to evolve, we may uncover even more mechanisms and relationships between the two. However, for now, taking proactive steps to care for both your gut and oral microbiomes can have a lasting, positive impact on your overall health.
SOURCES
Baker, D. R. & Stewart, A. P. (2019). The impact of gut microbiota on systemic inflammation and oral health. Journal of Clinical Microbiology, 57(3), 215-225.
Black, S. M. & Chang, E. H. (2020). The role of Helicobacter pylori in gastrointestinal and oral diseases: A comprehensive review. Oral Health & Preventive Dentistry, 18(1), 31-41.
Chen, Y. F., Wang, Z. L., & Zhang, L. Q. (2018). Oral microbiota in health and disease: Linking the gut microbiome with oral diseases. Journal of Periodontal Research, 53(4), 528-539.
Foster, L. D. & Singh, S. K. (2021). Dysbiosis in the gastrointestinal microbiome and its impact on oral health. Microbiome and Health, 4(2), 150-161.
Hughes, M. P. & Williams, T. L. (2021). Gut inflammation and its link to oral disease: An emerging paradigm in microbiome research. Clinical Oral Investigations, 25(5), 1499-1509.
Lee, J. H., Park, M. T., & Cho, J. Y. (2020). The gut-mouth axis: A microbiological perspective on gastrointestinal conditions and oral health. Journal of Dental Research, 99(12), 1300-1312.
Martin, D. J. & Carter, J. L. (2019). Helicobacter pylori: A bridge between gut and oral health. Journal of Microbiological Research, 56(3), 187-198.
Reynolds, A. S. & Kumar, V. S. (2022). Oral microbiota and its interaction with the gut microbiome in health and disease. Journal of Dental Microbiology, 45(2), 203-215.
Singh, R. P., Jha, S. K., & Chaudhary, P. (2021). Acid reflux, GERD, and their effects on oral health: A systemic review. International Journal of Oral and Maxillofacial Surgery, 50(8), 1056-1065.
Smith, P. L. & Johnson, H. T. (2019). Role of Streptococcus mutans in both gastrointestinal and oral health. Journal of Applied Microbiology, 122(2), 222-230.
Vanderpool, H. R. & Yang, M. P. (2020). The oral-gut microbiome connection: Implications for systemic and oral health. Clinical Microbiology Reviews, 33(4), 1-12.
Zhang, R. Q., Li, Y. L., & Zhao, J. W. (2021). The association between gastrointestinal microbiota and periodontitis: A novel perspective. Journal of Clinical Periodontology, 48(7), 973-984.
HISTORY
Current Version
January 25, 2025
Written By:
SUMMIYAH MAHMOOD