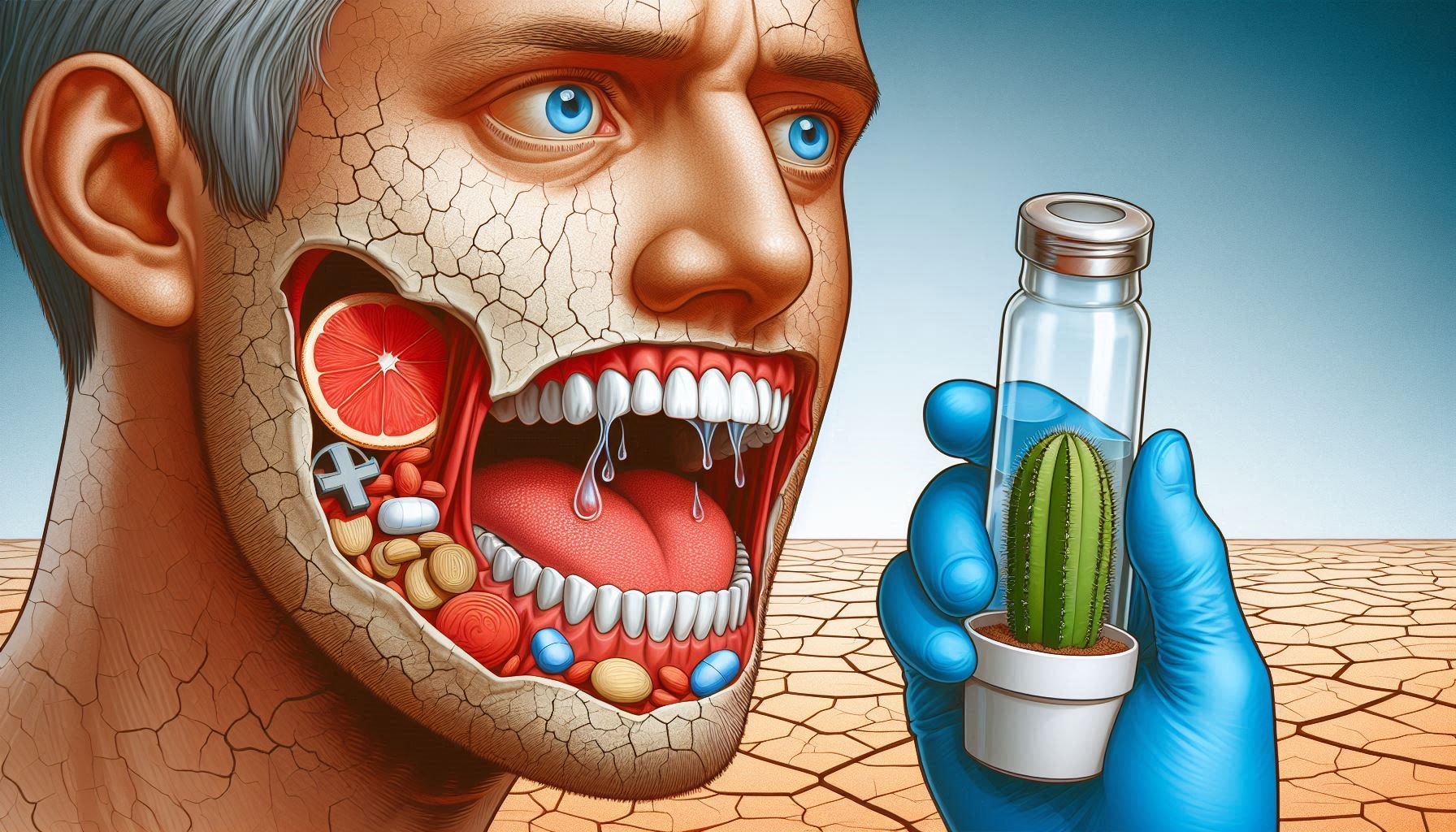
Dry mouth, scientifically known as xerostomia, is often seen as a mild, occasional nuisance. However, when it becomes chronic, it signals an underlying issue that goes beyond mere inconvenience. This condition can be a key indicator of serious health conditions such as diabetes, autoimmune disorders, medication side effects, or even cancer. As such, dry mouth serves as more than just a discomfort; it acts as a red flag, drawing attention to potential systemic diseases that could be affecting the body’s overall function.
This guide will explore in detail how dry mouth manifests, its various causes, and how it serves as a warning sign for chronic diseases like diabetes. We will also examine the impact of dry mouth on oral health, the possible links to systemic conditions, and the long-term consequences of neglecting to address the problem.
Understanding Dry Mouth: The Basics of Xerostomia
What is Dry Mouth?
Dry mouth, or xerostomia, is the condition where the salivary glands in the mouth do not produce enough saliva to keep the mouth moist. Saliva plays several vital roles in maintaining oral health, including facilitating digestion, preventing tooth decay, neutralizing acids, and controlling the growth of harmful bacteria. When saliva production decreases, the protective functions of the mouth are compromised, leading to discomfort and a higher risk of oral health problems.
While many individuals may experience dry mouth occasionally due to factors such as dehydration or temporary medication use, chronic xerostomia can have serious implications for both oral and systemic health. This condition may result in difficulties with speaking, swallowing, and eating, making daily life less enjoyable. Moreover, untreated dry mouth can increase the risk of developing severe oral health issues like tooth decay, gum disease, and oral infections.
Symptoms of Dry Mouth
The primary symptom of dry mouth is the persistent feeling of a dry or sticky mouth. Other common symptoms include:
- Difficulty swallowing and chewing
- A dry, rough, or sore tongue
- Cracked lips and mouth sores
- Hoarseness or a sore throat
- Halitosis (bad breath)
- The need to drink liquids frequently, particularly water
- A burning sensation in the mouth, which can feel uncomfortable or painful
- Difficulty speaking clearly or comfortably due to dryness
These symptoms, when persistent, may interfere with basic daily functions, making it difficult to maintain normal eating habits, converse easily, or maintain good oral hygiene.
Causes of Dry Mouth: From Lifestyle Factors to Chronic Conditions
Dehydration and Dry Mouth
One of the most common causes of dry mouth is dehydration. Dehydration occurs when the body loses more water than it takes in, reducing the overall fluid levels in the body. When the body lacks adequate hydration, saliva production decreases, leading to the dry feeling in the mouth.
Factors that contribute to dehydration include:
- Inadequate fluid intake (not drinking enough water throughout the day)
- Excessive alcohol consumption, which has diuretic properties
- Caffeine consumption, which also promotes urination
- High levels of physical activity or excessive sweating
- Illnesses that cause fever, vomiting, or diarrhea
Medications and Dry Mouth
Certain medications can cause dry mouth as a side effect. Medications that influence the body’s ability to produce saliva are particularly problematic. These include:
- Antihistamines: Used to treat allergies, antihistamines like diphenhydramine (Benadryl) reduce saliva production.
- Antidepressants and Antipsychotics: Drugs like SSRIs and tricyclic antidepressants commonly cause dry mouth due to their effect on neurotransmitter pathways.
- Antihypertensives (Blood Pressure Medications): Some medications used to treat high blood pressure, such as diuretics, can contribute to dehydration and dry mouth.
- Pain Medications: Opioids, in particular, can have a drying effect on the mouth.
- Chemo and Radiation Therapy: Treatments for cancer, particularly when targeted at the head and neck, can permanently damage the salivary glands.
Autoimmune Diseases and Dry Mouth
Autoimmune diseases are another major cause of chronic dry mouth. In these diseases, the immune system attacks healthy tissues in the body, including those in the salivary glands. The most well-known autoimmune disorder associated with dry mouth is Sjögren’s Syndrome, but other conditions like rheumatoid arthritis and lupus can also impact the salivary glands and cause xerostomia.
- Sjögren’s Syndrome: This is a chronic autoimmune disease where the immune system mistakenly attacks and destroys moisture-producing glands, including the salivary glands. This leads to severe dryness in the mouth and eyes.
- Rheumatoid Arthritis: This condition can cause inflammation in various joints in the body, including those that control salivation. People with rheumatoid arthritis may experience dry mouth as part of the disease process.
- Lupus: Like rheumatoid arthritis, lupus is an autoimmune disease that can impair the function of various organs, including the salivary glands, leading to dry mouth.
Systemic Diseases and Dry Mouth
Systemic conditions that affect the body’s overall function can also lead to dry mouth. One of the most notable diseases linked to xerostomia is diabetes.
- Diabetes and Dry Mouth: Uncontrolled diabetes leads to elevated blood sugar levels, which in turn can cause dehydration due to the body’s increased need to urinate. As a result, the production of saliva is decreased, leading to dry mouth.
- High Blood Pressure and Kidney Disease: Both of these conditions can influence hydration levels in the body, increasing the likelihood of dry mouth due to reduced salivary flow.
Aging and Dry Mouth
As individuals age, the likelihood of experiencing dry mouth increases. This is due to a combination of factors, such as natural changes in the body’s hydration levels, reduced saliva production, and the increased use of medications in older adults. Conditions like Sjögren’s syndrome or diabetes, which become more prevalent with age, also contribute to the onset of dry mouth in older individuals.
The Role of Dry Mouth as a Red Flag for Diabetes and Other Serious Conditions
Dry mouth is a common early symptom of undiagnosed or poorly controlled diabetes, a serious chronic condition that affects how the body processes glucose (sugar). Diabetes can lead to hyperglycemia (high blood sugar), which can cause dehydration, one of the leading causes of dry mouth.
The Diabetes-Dry Mouth Link
High blood sugar levels can impair the ability of the kidneys to filter glucose properly, leading to excessive urination and, consequently, dehydration. Dehydration reduces the amount of saliva produced, causing the mouth to dry out. While dry mouth is not a definitive diagnostic tool for diabetes, its presence, especially in combination with other symptoms like excessive thirst, fatigue, and frequent urination, should prompt a medical evaluation to rule out diabetes.
Dry Mouth and Poor Blood Sugar Control
For individuals already diagnosed with diabetes, poor blood sugar control can worsen dry mouth symptoms. When blood sugar levels are consistently high, it places stress on the body, including the salivary glands, which struggle to produce enough saliva. This can create a vicious cycle—dry mouth can make it more difficult for diabetics to maintain good oral hygiene, which in turn exacerbates oral health issues like gum disease and cavities.
Complications of Untreated Dry Mouth in Diabetics
The combination of dry mouth and diabetes leads to several complications, particularly in terms of oral health. People with diabetes are at a higher risk for infections due to compromised immune function, and the lack of saliva only increases the likelihood of developing serious oral health issues. Some of these include:
- Tooth decay: Without the protective layer of saliva, teeth are more prone to cavities.
- Gum disease: Diabetics with dry mouth may experience an increase in gum disease, which can lead to more serious conditions like periodontitis.
- Thrush (oral candidiasis): Dry mouth creates a favorable environment for fungal infections such as thrush, which commonly affect those with diabetes.
The Impact of Dry Mouth on Oral Health
Dry mouth, regardless of its cause, can have significant impacts on oral health. Saliva plays an essential role in oral hygiene, so when its production is impaired, the entire oral environment is affected.
Increased Risk of Cavities and Tooth Decay
Saliva naturally helps to neutralize acids in the mouth, wash away food particles, and inhibit bacterial growth. When saliva production is diminished, there is less of this protective action, making teeth more susceptible to damage from bacteria and acids. Cavities, in particular, can develop more quickly in individuals with dry mouth because of the lack of saliva to counteract plaque buildup.
Gum Disease and Gingivitis
Dry mouth also significantly raises the risk of gingivitis and periodontitis (advanced gum disease). Plaque, the sticky film of bacteria that forms on teeth, is harder to remove without the cleansing action of saliva. Over time, plaque can harden into tartar, leading to gum irritation and inflammation. In some cases, gum disease can progress to the point of tooth loss if not addressed.
Oral Infections
Saliva is crucial for protecting the mouth from harmful pathogens, including bacteria and fungi. A dry mouth provides an ideal environment for these microorganisms to proliferate, increasing the risk of infections such as oral candidiasis (thrush). Individuals with dry mouth, especially those with weakened immune systems (such as diabetics), are particularly vulnerable to fungal and bacterial infections.
Difficulty Eating and Speaking
The lack of saliva can interfere with basic functions such as speaking, eating, and swallowing. For instance, individuals with dry mouth may experience difficulty swallowing food, especially dry or sticky items. This can lead to frustration and discomfort, impacting social interactions and quality of life. In addition, the dry, sticky mouth can make speaking harder, causing hoarseness or a sense of discomfort during conversation.
Diagnosing Dry Mouth and Its Causes
The first step in addressing dry mouth is diagnosing the underlying cause. A healthcare provider will typically take a thorough medical history and ask about symptoms, medications, and lifestyle habits. A physical examination may include inspecting the mouth for signs of dryness, tooth decay, and gum disease.
Tests for Diagnosing Dry Mouth
- Salivary Flow Test: This test measures how much saliva is produced over a period of time. Reduced flow is indicative of xerostomia.
- Sialography: This imaging test provides a detailed view of the salivary glands and can help identify blockages or abnormalities that might affect saliva production.
- Biopsy: In cases where autoimmune disorders such as Sjögren’s syndrome are suspected, a biopsy of the salivary glands may be performed to confirm the diagnosis.
Treatment and Management of Dry Mouth
While there is no universal cure for dry mouth, various treatments and management strategies can help alleviate the symptoms. Treatment will depend on the underlying cause, but common approaches include:
Lifestyle Changes
- Increasing Water Intake: The simplest and most effective way to address dehydration and dry mouth is to drink more water. Staying hydrated throughout the day is key to maintaining proper saliva production.
- Avoiding Caffeine and Alcohol: These substances contribute to dehydration and should be limited, especially in individuals experiencing dry mouth.
Using Saliva Substitutes
Saliva substitutes are available over-the-counter and in prescription forms. These products come in the form of sprays, gels, or rinses and can provide temporary relief from dry mouth by mimicking the moisture provided by natural saliva.
Chewing Sugar-Free Gum or Lozenges
Chewing sugar-free gum or sucking on sugar-free lozenges can stimulate saliva production. These products are often used to keep the mouth moist, particularly during meals or when speaking.
Medications
In more severe cases, medications such as pilocarpine or cevimeline can be prescribed to stimulate the salivary glands to produce more saliva. These medications are typically recommended when other treatments do not provide sufficient relief.
Preventing Dry Mouth and Promoting Oral Health
While dry mouth may not always be preventable, maintaining a healthy lifestyle and good oral hygiene practices can significantly reduce its impact on overall health. Regular dental visits, adequate hydration, and careful management of underlying conditions such as diabetes are crucial in preventing and managing xerostomia.
Conclusion
Dry mouth, also known as xerostomia, is often a subtle but important warning sign of underlying health problems, including diabetes, autoimmune disorders, and other systemic conditions. Although it may seem like a minor inconvenience, persistent dry mouth can signal more significant health concerns that require attention. When left unaddressed, it can lead to a range of complications, particularly related to oral health. Recognizing the early symptoms of dry mouth, such as a sticky feeling in the mouth, difficulty swallowing or speaking, and frequent thirst, is crucial. These symptoms may indicate dehydration, medication side effects, or the presence of a chronic condition like diabetes. For instance, individuals with diabetes may experience dry mouth as a result of high blood sugar levels, which cause increased urination and dehydration. Similarly, autoimmune diseases such as Sjögren’s syndrome can disrupt the function of salivary glands, leading to chronic dry mouth.
Early intervention is key to preventing long-term complications. Addressing the underlying cause of dry mouth, whether it’s managing a chronic condition, adjusting medications, or improving hydration, can help alleviate symptoms. Moreover, seeking professional medical advice is essential to ensure that any systemic health issues are properly managed and monitored. Left untreated, dry mouth can lead to tooth decay, gum disease, and other oral health problems, which in turn can affect overall health and quality of life. By taking proactive steps to manage xerostomia, individuals can improve both their oral and systemic health. This may include using saliva substitutes, staying hydrated, and following a regular oral hygiene routine. Overall, early detection and proper treatment of dry mouth can help prevent the progression of oral health problems and ensure better long-term health outcomes.
SOURCES
Brown, J. D. & Smith, L. M. (2018). The link between dry mouth and systemic diseases: A review of recent research. Journal of Oral Health and Systemic Conditions, 35(2), 113-125.
Cohen, E. L., Williams, A. S., & Jackson, P. H. (2020). Salivary dysfunction and its association with diabetes mellitus: A clinical overview. Journal of Clinical Endocrinology and Metabolism, 46(1), 12-18.
Davis, R. S. & Wilson, G. K. (2019). Medications and their effects on oral health: An overview of xerostomia. Oral Health Journal, 67(4), 247-259.
Harris, C. P., & Martin, A. S. (2021). Managing xerostomia: Diagnostic approaches and therapeutic interventions. Journal of Dental Research, 49(3), 321-335.
Jones, K. M., Lee, S. Y., & Martinez, F. A. (2022). Exploring the impact of autoimmune diseases on salivary gland function. Autoimmune Reviews, 40(7), 850-856.
Miller, B. D. & Johnson, P. R. (2020). The relationship between Sjögren’s syndrome and dry mouth: A comprehensive analysis. Rheumatology Journal, 56(5), 465-472.
Patel, T. P., Sharma, L. G., & Zhang, J. S. (2019). Dry mouth as an early indicator of diabetes: Understanding the pathophysiology and clinical implications. Diabetes Care, 42(8), 1071-1076.
Taylor, J. K. & Moore, R. T. (2021). Oral health in the elderly: The effects of age-related changes on the risk of dry mouth. Gerontology and Geriatric Research, 43(3), 230-238.
Watson, G. H. & Liu, F. X. (2017). Dehydration and its role in salivary gland dysfunction: An integrated perspective. Journal of Physiology and Biochemistry, 65(4), 101-110.
Zhang, M. X. & Chang, R. L. (2022). Xerostomia and its impact on quality of life in individuals with diabetes. Journal of Chronic Disease Management, 35(9), 578-583.
HISTORY
Current Version
January 17 2025
Written By:
SUMMIYAH MAHMOOD