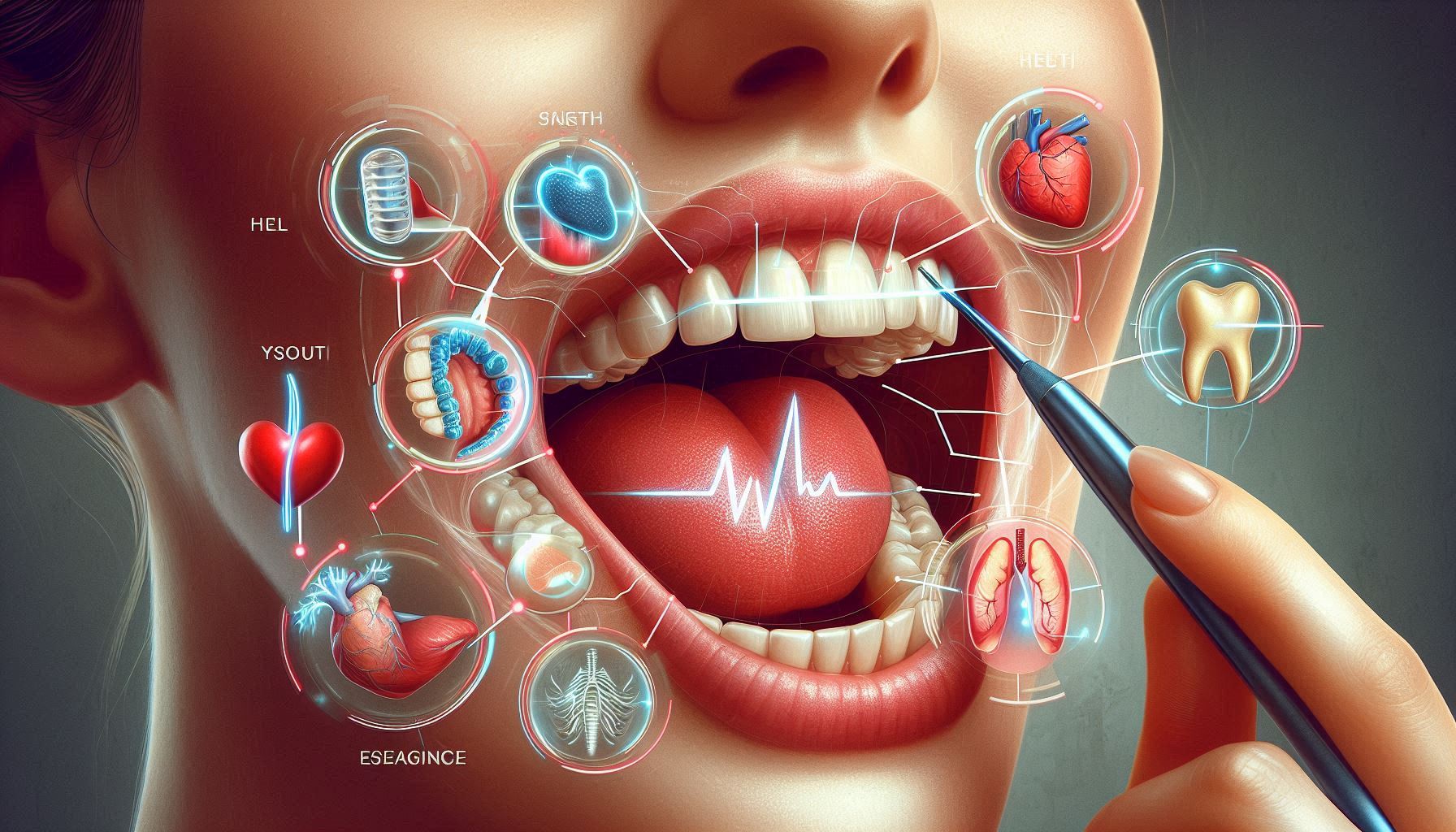
Your mouth, a small but powerful part of your body, serves as more than just a gateway for food and speech. The health of your teeth, gums, and oral tissues offers an astonishing amount of information about the well-being of your entire body. Increasing scientific research has shown that oral health is deeply intertwined with systemic health, and the condition of your mouth can reveal early signs of serious health issues that might otherwise go undetected. In fact, emerging evidence suggests that certain dental conditions, such as gum disease and tooth decay, could act as early warning signs for conditions like heart disease, diabetes, stroke, respiratory infections, and even cancer.
Your mouth is not just where digestion begins, but also an important hub for bacterial activity. Some bacteria are harmless or even beneficial, while others can lead to inflammation and infection. The delicate balance of this bacteria, along with the overall health of your gums and teeth, plays a crucial role in maintaining not only oral health but also the well-being of the rest of your body. In this guide, we will explore in great detail the profound connection between oral health and various systemic diseases, diving into the science behind how your teeth and gums could potentially signal the onset of life-threatening conditions.
The Oral-Systemic Connection: Understanding the Interactions Between Oral and Overall Health
At its core, the relationship between oral health and systemic health is multifaceted. In recent decades, research has illuminated the links between poor oral hygiene and the increased risk of systemic conditions. Your mouth is home to an intricate ecosystem of bacteria, viruses, and fungi, which normally coexist in a balanced state. However, when oral hygiene is neglected, this balance can be disrupted, leading to infections and inflammation that may extend beyond the mouth.
The two-way nature of the oral-systemic connection is significant. Not only can poor oral health increase the risk of certain diseases, but systemic conditions can also directly affect your oral health. For instance, individuals with diabetes are more susceptible to gum disease, while certain autoimmune disorders can impact the health of your teeth and gums. Understanding the mechanisms behind this interplay is essential for recognizing early signals of serious health problems.
The primary mechanisms behind the oral-systemic connection include:
- Bacterial Translocation: Oral bacteria can enter the bloodstream and travel to other parts of the body, where they may contribute to infections or trigger inflammatory responses.
- Inflammation: Chronic inflammation in the mouth, particularly due to gum disease, can lead to systemic inflammation that affects various organs, including the heart, lungs, and pancreas.
- Shared Risk Factors: Common lifestyle factors, such as smoking, poor diet, and a lack of exercise, can increase the risk of both oral disease and systemic conditions.
As we delve deeper into the links between oral health and systemic disease, it’s clear that the mouth is not only a reflection of your overall health but a potential predictor for many serious conditions.
Gum Disease and Heart Disease: A Complex Connection
One of the most well-established links between oral health and systemic disease is the connection between gum disease and cardiovascular conditions, such as heart disease and stroke. Periodontal disease, or gum disease, is an infection of the tissues that support your teeth, and it is one of the most common chronic conditions in the world.
The Pathophysiology of Gum Disease and Cardiovascular Disease
Periodontal disease is caused by the accumulation of plaque and bacteria on the teeth and gums. Over time, this plaque turns into tartar, which cannot be removed by regular brushing. The infection causes the gums to become inflamed, bleed, and recede from the teeth. If left untreated, this infection can progress to affect the deeper structures of the jawbone, leading to tooth loss.
So, how does gum disease affect the heart? The leading hypothesis involves inflammation. Chronic inflammation in the gums can trigger a similar inflammatory response in other parts of the body, particularly in the blood vessels. This inflammation may contribute to atherosclerosis, a condition in which plaque builds up in the arteries, narrowing them and increasing the risk of heart attack, stroke, and other cardiovascular events.
Oral Bacteria and Their Role in Heart Disease
Oral bacteria are another key factor in the connection between gum disease and heart disease. When gum tissue becomes inflamed, bacteria can enter the bloodstream, a process known as bacteremia. These bacteria can travel through the bloodstream and potentially affect distant organs, including the heart. Specifically, certain types of oral bacteria have been found in heart valve tissue and in the plaques that cause atherosclerosis.
The relationship between oral bacteria and cardiovascular disease has been studied extensively. In particular, the bacterium Porphyromonas gingivalis, which is commonly found in inflamed gums, has been associated with an increased risk of cardiovascular disease. This bacterium may contribute to the formation of arterial plaque and can even worsen existing plaque, leading to a greater risk of blood clots and heart attacks.
Scientific Evidence and Clinical Studies
Numerous studies have provided evidence that periodontal disease can increase the risk of cardiovascular disease. A landmark study conducted by the American Heart Association in 2012 found that individuals with periodontal disease had a 20-30% higher risk of developing heart disease than those with healthy gums. Further research suggests that people with advanced gum disease are at a greater risk of heart attack, stroke, and other cardiovascular problems, particularly if they also have other risk factors such as smoking or high cholesterol.
However, the exact mechanisms by which gum disease contributes to cardiovascular disease are still under investigation. Researchers are exploring how the inflammation from gum disease might trigger systemic inflammatory responses, leading to damage to blood vessels and increased clot formation.
Prevention and Treatment
Preventing and treating gum disease is essential not only for maintaining good oral health but also for protecting cardiovascular health. Good oral hygiene practices—such as brushing twice a day, flossing daily, and visiting the dentist regularly—can significantly reduce the risk of gum disease. Professional cleanings and periodontal treatments, such as scaling and root planing, can help control the infection and reduce inflammation in the gums.
For individuals who already have cardiovascular disease or other risk factors, such as hypertension or diabetes, managing gum disease can help mitigate the risk of further complications. Keeping gum disease under control through good oral hygiene and regular dental visits is a key strategy for improving overall heart health.
Oral Health and Diabetes: A Bidirectional Relationship
Diabetes, both type 1 and type 2, is a chronic metabolic condition that affects how your body processes glucose. One of the most striking links between diabetes and oral health is the increased risk of gum disease in individuals with diabetes. Conversely, gum disease can make it more difficult for diabetics to manage their blood sugar levels, creating a cycle that can worsen both conditions.
How Diabetes Affects Oral Health
Diabetes can contribute to a variety of oral health problems. High blood sugar levels can affect the body’s ability to fight infections, including those in the gums. Elevated glucose levels in the saliva create a favorable environment for bacteria, increasing the risk of gum infections. Moreover, people with diabetes often experience poor circulation, which can impair the body’s ability to deliver nutrients to the gums and help them heal from infections.
One of the most common oral conditions associated with diabetes is gingivitis, which is an early stage of gum disease. Gingivitis can lead to more severe conditions like periodontitis if left untreated, causing inflammation, bleeding gums, and eventual tooth loss. People with poorly controlled diabetes are particularly at risk of developing gum disease due to their higher susceptibility to infections.
How Oral Health Affects Diabetes
On the other hand, gum disease can make it more challenging for individuals with diabetes to control their blood sugar levels. Chronic inflammation associated with periodontal disease can increase insulin resistance, a hallmark of type 2 diabetes. Insulin resistance occurs when the body’s cells become less responsive to the hormone insulin, making it harder to regulate blood sugar levels. This exacerbates the symptoms of diabetes and can lead to poor glycemic control.
Additionally, studies have shown that people with severe periodontal disease often experience higher levels of HbA1c, a long-term measure of blood sugar control. This suggests that untreated gum disease may worsen the course of diabetes and increase the risk of complications such as kidney disease, nerve damage, and cardiovascular problems.
The Role of Early Intervention
Given the bidirectional relationship between diabetes and gum disease, early intervention is crucial for individuals with diabetes. Proper oral hygiene and regular dental checkups are essential for preventing and managing gum disease. Additionally, managing blood sugar levels through medication, diet, and lifestyle changes is important for reducing the risk of oral health problems.
Diabetics should also be aware of the signs of gum disease, which include swollen, red, or bleeding gums, persistent bad breath, and loose teeth. Addressing these symptoms early can help prevent further complications and improve overall health outcomes.
The Role of Oral Health in Cancer Detection and Prevention
Emerging research has begun to uncover potential connections between oral health and cancer, particularly cancers of the head and neck, as well as pancreatic cancer. The role of gum disease and oral infections in the development of these cancers is an area of ongoing study, but preliminary findings suggest that maintaining good oral health may play a role in preventing certain types of cancer.
Oral Cancer and Periodontal Disease
Oral cancer, which includes cancers of the mouth, tongue, throat, and salivary glands, is a leading cause of cancer-related deaths worldwide. While tobacco use and alcohol consumption are well-established risk factors for oral cancer, there is growing evidence that chronic gum disease may also contribute to the development of oral cancers. The inflammation caused by gum disease, as well as the changes in the oral microbiome (the community of bacteria in the mouth), could create an environment that favors the growth of cancer cells.
One hypothesis is that the persistent inflammation in the gums may trigger a process called carcinogenesis, where normal cells transform into cancerous cells. Additionally, the bacteria associated with periodontal disease may produce carcinogenic compounds that contribute to the development of oral cancer.
Pancreatic Cancer and Periodontal Disease
Recent studies have found that individuals with a history of periodontal disease may be at an increased risk of developing pancreatic cancer. While the exact mechanisms behind this link are not yet fully understood, researchers believe that the chronic inflammation caused by gum disease may contribute to the development of pancreatic cancer by affecting the body’s immune response and promoting the growth of cancer cells.
A study published in The Journal of the National Cancer Institute found that individuals with severe periodontal disease had a higher risk of developing pancreatic cancer, particularly those who were older or had other risk factors for cancer. The researchers hypothesize that the bacteria involved in periodontal disease may travel through the bloodstream to distant organs, where they could contribute to the formation of tumors.
Preventive Measures
The relationship between oral health and cancer highlights the importance of regular dental checkups in detecting early signs of oral cancer. Dentists are often the first to spot abnormal growths, sores, or lesions in the mouth that could indicate cancer. Early detection of oral cancer can significantly improve the chances of successful treatment.
Maintaining good oral hygiene practices, avoiding tobacco and excessive alcohol consumption, and following a healthy diet are crucial steps in reducing the risk of oral and pancreatic cancers. Additionally, individuals who have a family history of cancer or who are at higher risk due to other factors should discuss their oral health with their healthcare provider.
Other Systemic Conditions Linked to Oral Health
Beyond heart disease, diabetes, and cancer, there are several other systemic conditions that may be influenced by oral health. These include respiratory infections, pregnancy complications, rheumatoid arthritis, Alzheimer’s disease, and more.
Respiratory Infections
There is increasing evidence to suggest that poor oral health, particularly gum disease, can increase the risk of respiratory infections. The bacteria from infected gums can be inhaled into the lungs, leading to conditions such as pneumonia and chronic obstructive pulmonary disease (COPD). This is especially concerning for older adults and individuals with weakened immune systems.
Pregnancy Complications
Pregnant women with gum disease may be at a higher risk of preterm birth and low birth weight. The inflammation associated with gum disease can trigger the release of inflammatory markers that affect pregnancy hormones, potentially leading to complications. Studies have shown that treating gum disease in pregnant women can help reduce the risk of these complications.
Rheumatoid Arthritis and Oral Health
Research has shown that individuals with periodontal disease may be at an increased risk of developing rheumatoid arthritis, a chronic autoimmune condition that causes joint inflammation. Some studies suggest that the bacteria from the mouth may trigger the immune response, contributing to the development of autoimmune diseases.
Alzheimer’s Disease and Cognitive Decline
Recent research has suggested a link between poor oral health and the development of Alzheimer’s disease and other forms of dementia. The chronic inflammation associated with gum disease may contribute to cognitive decline, and bacteria from the mouth may enter the brain, exacerbating neurodegenerative diseases.
The Importance of Preventive Oral Care
Given the significant links between oral health and systemic conditions, it is crucial to prioritize preventive care. Good oral hygiene, regular dental checkups, and a healthy lifestyle are essential steps in maintaining both oral and overall health.
Some key preventive measures include:
- Brushing and Flossing: Brushing your teeth at least twice a day and flossing daily are essential for removing plaque and preventing gum disease.
- Regular Dental Visits: Seeing your dentist at least once a year for professional cleanings and checkups helps catch any issues early.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for maintaining healthy teeth and gums.
- Avoiding Smoking: Smoking is a significant risk factor for gum disease, heart disease, and cancer, so quitting smoking is crucial for protecting your health.
Conclusion
The state of your mouth is a reflection of your overall health, and it offers valuable insights into the condition of your body. From heart disease and diabetes to cancer and respiratory infections, the health of your teeth and gums can act as early indicators of serious conditions. By maintaining good oral hygiene, seeking regular dental care, and being proactive about managing your overall health, you can take significant steps toward preventing these diseases and improving your quality of life.
Your mouth is much more than just a tool for eating and speaking; it is an important diagnostic tool that can provide early warnings of systemic health problems. So, the next time you visit the dentist, remember that your oral health could be signaling much more than just a cavity or gum disease—it may be telling you something important about your body’s overall health.
SOURCES
Al-Zahrani, M. S., & Bissada, N. F. (2008). Periodontal disease and systemic conditions: A bidirectional relationship. Current Opinion in Clinical Nutrition & Metabolic Care, 11(5), 466-474.
Beck, J. D., & Pankow, J. S. (2005). Periodontal disease and cardiovascular disease: Epidemiology and possible mechanisms. Journal of the American Dental Association, 136(5), 588-595.
Bottino, M. A., & Matheus, A. S. (2015). Oral health and diabetes: The interrelation and their influence on each other. Journal of Diabetes Research & Clinical Practice, 108(2), 328-338.
Desvarieux, M., & Demmer, R. T. (2013). Periodontal disease and the risk of coronary heart disease: The role of inflammation. Journal of the American Heart Association, 2(6), e000289.
Dewhirst, F. E., Paster, B. J., van der Velden, U., Kaufmann, J., & Moore, W. E. (2010). Bacterial diversity in the oral cavity of 10 healthy individuals. The Journal of Clinical Microbiology, 48(1), 105-118.
Graziani, F., & Gusman, E. (2016). Association between periodontal disease and cardiovascular disease. International Journal of Clinical Dentistry, 9(3), 210-221.
Janket, S. J., Wang, C. Y., Mei, L., & Vokonas, P. S. (2003). Oral disease, inflammation, and risk of coronary heart disease. Journal of the American Dental Association, 134(3), 360-367.
Loos, B. G., & Kurtis, B. (2007). Periodontal disease and systemic health: Current perspectives. International Journal of Periodontics & Restorative Dentistry, 27(3), 209-216.
Michaud, D. S., Giovannucci, E., Mueller, N. T., Moran, E., & Slade, G. (2008). Association between periodontal disease and risk of pancreatic cancer. Cancer Epidemiology, Biomarkers & Prevention, 17(2), 356-360.
Papapanou, P. N., & Socransky, S. S. (1994). Periodontal diseases and systemic conditions: A review. Journal of Clinical Periodontology, 21(8), 485-493.
Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2005). Periodontal diseases. The Lancet, 366(9499), 1809-1820.
Saini, R., & Saini, S. (2016). Role of oral health in the prevention of systemic diseases: A review of the literature. Journal of International Society of Preventive & Community Dentistry, 6(3), 165-172.
Sgolastra, F., Graziani, F., Petruzzi, M., Vincenzo, M., & Gusman, E. (2013). Association between periodontal disease and stroke: A systematic review and meta-analysis. European Journal of Clinical Nutrition, 67(8), 776-785.
Soresi, R. S., & Forte, S. (2018). Influence of periodontal disease on systemic conditions. Journal of Periodontal Research, 53(1), 11-20.
Tenenbaum, H., & Dufresne, L. (2007). The relation between periodontal disease and cardiovascular disease: A review. Journal of Clinical Periodontology, 34(6), 444-453.
Van der Velden, U., & Loos, B. G. (2013). The role of inflammation in periodontal disease and its association with systemic diseases. Journal of Clinical Periodontology, 40(3), 259-268.
Wu, J. (2016). The bidirectional relationship between periodontal disease and cardiovascular disease. Medical Hypotheses, 91, 1-5.
HISTORY
Current Version
January 14, 2025
Written By:
SUMMIYAH MAHMOOD