Chronic acid reflux, also known as gastroesophageal reflux disease (GERD), is a condition that affects millions of people around the world. It occurs when stomach acid or bile irritates the food pipe lining, leading to frequent heartburn and acid regurgitation. While the most common symptoms of acid reflux are digestive, such as heartburn, regurgitation, and chest pain, the effects of GERD can extend beyond the digestive system, impacting other parts of the body, including the teeth. Over time, chronic acid reflux can have significant consequences for oral health, leading to various dental problems that can impact the appearance, function, and overall health of your teeth.
This guide explores in-depth the impact of chronic acid reflux on dental health. It covers the mechanisms behind acid reflux, the specific effects on teeth, the long-term consequences of untreated acid reflux, and ways to prevent and manage these dental issues.
Understanding Acid Reflux and GERD
To appreciate how chronic acid reflux affects your teeth, it is essential to first understand what acid reflux and GERD are and how they work. Acid reflux occurs when the lower esophageal sphincter (LES), a ring of muscle at the junction between the esophagus and stomach, fails to close properly. When this happens, stomach acid can flow back up into the esophagus, causing irritation and inflammation. If acid reflux happens more than twice a week, it is classified as GERD, a more severe and chronic form of reflux.
The stomach’s acidic environment is necessary for digestion and breaking down food. However, the lining of the stomach is protected from the harmful effects of acid by a thick mucosal layer. In contrast, the lining of the esophagus, as well as the mouth and teeth, is not equipped to handle exposure to such acidity.
The Mechanism Behind Acid Reflux’s Effect on Teeth
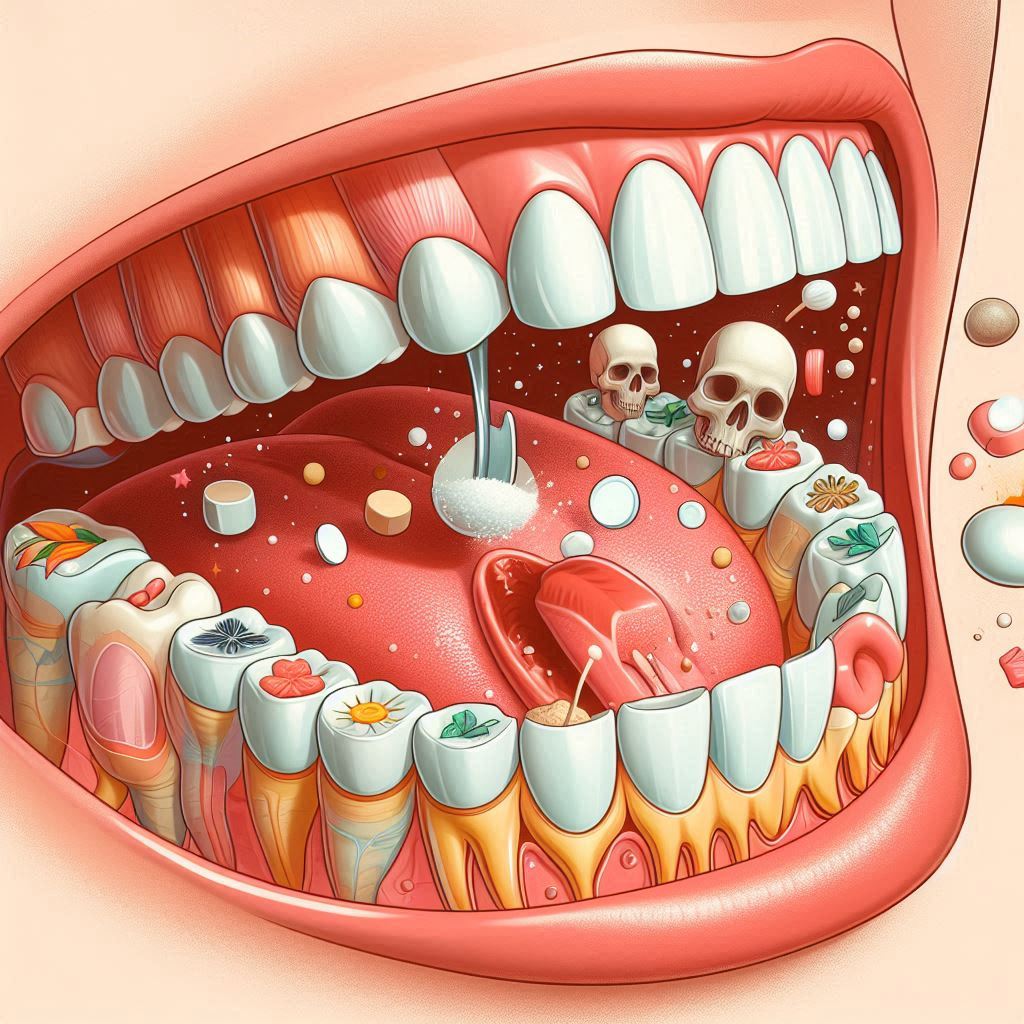
When stomach acid regurgitates into the mouth, it can lead to several dental issues. This is primarily due to the highly acidic nature of stomach contents, which can be as low as pH 1.5 to 3.5, which is similar to the acidity of battery acid. When this acid reaches the mouth, it can interact with the teeth, leading to enamel erosion.
The enamel is the outermost layer of the teeth, providing protection against decay and damage. It is the hardest tissue in the human body, but it is also vulnerable to acid attacks. When stomach acid comes into contact with the enamel, it begins to break down the minerals that make up the tooth structure, especially calcium. This process is known as demineralization. Over time, repeated exposure to acid weakens the enamel, causing it to thin, wear down, and become more susceptible to cavities, sensitivity, and other oral health issues.
Additionally, acid reflux can cause dry mouth (xerostomia) due to a decrease in saliva production. Saliva plays a critical role in neutralizing acids in the mouth and promoting remineralization of teeth. Without adequate saliva, the natural defense mechanism against tooth erosion is compromised, making the teeth more vulnerable to the effects of acid reflux.
3. Common Dental Problems Associated with Chronic Acid Reflux
There are several dental complications that are commonly associated with chronic acid reflux. Below are some of the most prevalent problems seen in individuals suffering from GERD.
3.1. Enamel Erosion
Enamel erosion is the most direct and noticeable effect of chronic acid reflux on teeth. The enamel, when exposed to stomach acid, begins to demineralize, which leads to thinning and weakening of the enamel. As the enamel erodes, the underlying dentin layer becomes exposed. Dentin is softer and more sensitive, which can result in tooth sensitivity. The erosion of enamel can also lead to a loss of tooth structure, causing teeth to appear smaller, more rounded, and less aesthetically pleasing.
Enamel erosion due to acid reflux typically manifests in a distinct pattern:
- Posterior Teeth: The backs of the upper molars are the most affected because they are the first to come into contact with regurgitated stomach acid. The enamel here can become thinner, causing the teeth to lose their shine and appear dull.
- Incisors and Premolars: In some cases, the front teeth (incisors) and premolars may also show signs of erosion due to repeated exposure to acid.
- Aesthetic Changes: As enamel wears away, the underlying dentin, which is naturally yellowish in color, becomes exposed, giving the teeth a yellowish hue.
3.2. Tooth Sensitivity
As enamel thins, it exposes the sensitive dentin underneath. The dentin is composed of microscopic tubules that lead directly to the nerve of the tooth. When these tubules are exposed to hot, cold, sweet, or acidic foods, they trigger sharp pain or discomfort, a condition known as tooth sensitivity. For individuals with chronic acid reflux, tooth sensitivity can become a daily issue, especially when eating or drinking acidic foods like citrus, coffee, or ice cream.
3.3. Cavities and Decay
The erosion of enamel leaves the dentin more vulnerable to bacterial invasion. The softer dentin can more easily absorb food particles, creating a breeding ground for harmful bacteria. The bacteria in the mouth feed on sugar and food debris, producing acids that further demineralize the tooth structure, ultimately leading to cavities. This process can be accelerated in individuals with acid reflux due to the constant acidic environment created by stomach acid.
3.4. Bad Breath (Halitosis)
Bad breath, or halitosis, is a common issue for individuals with acid reflux. When stomach acid regurgitates into the mouth, it can mix with food particles and bacteria to produce foul-smelling gases. The acid itself can also alter the pH balance of the mouth, encouraging the growth of odor-causing bacteria. Moreover, acid reflux can lead to dry mouth, reducing the saliva needed to wash away bacteria and food particles, further contributing to bad breath.
Discoloration
Enamel erosion can lead to discoloration of the teeth. As the enamel thins, the dentin underneath, which is naturally yellowish in color, can become more visible. This can give the teeth a yellowish or dull appearance. In addition, the acids from reflux can contribute to staining over time, further impacting the overall appearance of the teeth.
3.5. Gum Disease and Recession
While enamel erosion is the most obvious effect of chronic acid reflux, it can also indirectly contribute to gum disease and recession. Acid exposure can irritate the gums, causing inflammation and weakening the gum tissue. Over time, this can lead to gum recession, where the gums pull away from the teeth, exposing the sensitive root surfaces. Gum recession not only makes teeth more prone to decay but also increases the risk of periodontitis, a more severe form of gum disease.
4. Long-Term Effects of Chronic Acid Reflux on Oral Health
If acid reflux is left untreated, the cumulative effects on your teeth can be severe and long-lasting. As the enamel continues to erode, the teeth become weaker, more sensitive, and more prone to decay. In some cases, the damage may be so extensive that restorative dental treatments, such as fillings, crowns, or veneers, are required to restore the function and appearance of the teeth.
The long-term consequences of untreated acid reflux can also extend beyond individual teeth. Over time, widespread enamel erosion can lead to changes in the bite and the overall alignment of the teeth. This can result in difficulties with chewing, speaking, and maintaining proper oral hygiene.
Moreover, untreated acid reflux may exacerbate existing dental issues, such as gum disease or tooth decay, and contribute to more severe complications like tooth loss. In severe cases, the overall health of the mouth and teeth can deteriorate to the point where extensive dental procedures, such as tooth extractions or full mouth reconstruction, may be necessary.. Below are some potential long-term effects of chronic acid reflux on the teeth:
4.1. Tooth Loss
In the most severe cases of enamel erosion, the structural integrity of the teeth can be significantly weakened, leading to tooth fractures or even tooth loss. While enamel cannot regenerate, the dentin and other tissues in the tooth may continue to deteriorate as well, making the teeth more fragile and susceptible to damage. Tooth loss from acid reflux is not immediate but can become a gradual consequence over time.
4.2. Bite Changes and Malocclusion
As the teeth wear down from acid reflux, the bite may become misaligned. Enamel loss and changes in tooth structure can affect how the teeth come together, leading to bite problems such as malocclusion (misalignment of teeth). Malocclusion can cause discomfort, difficulty chewing, and even jaw pain. It may also affect the aesthetics of the smile.
4.3. Increased Risk of Periodontal Disease
Chronic acid reflux, in conjunction with poor oral hygiene, can increase the risk of periodontal disease. Periodontal disease is an infection of the gums and supporting structures of the teeth. As the gums become inflamed and recede due to acid exposure, they may become more susceptible to bacterial infections, leading to gum disease and, eventually, tooth loss if untreated.
5. Prevention and Management Strategies
While chronic acid reflux can cause significant damage to dental health, there are proactive steps individuals can take to mitigate these effects. The following strategies focus on preventing further dental damage and managing the condition effectively.
5.1. Managing Acid Reflux
The first line of defense against dental damage from acid reflux is to manage the reflux itself. This may involve:
- Dietary Modifications: Avoiding foods and beverages that trigger acid reflux, such as spicy foods, citrus, chocolate, caffeinated drinks, and fatty meals.
- Weight Management: Maintaining a healthy weight can reduce pressure on the stomach, helping to prevent acid reflux.
- Medications: Antacids, proton pump inhibitors (PPIs), and H2 blockers are commonly prescribed to reduce stomach acid production and prevent reflux episodes.
- Elevating the Head During Sleep: Sleeping with the head raised can help prevent acid from traveling back into the esophagus during the night.
5.2. Rinsing with Water
After an acid reflux episode, it is beneficial to rinse the mouth with water to help wash away stomach acid and neutralize the pH in the mouth. Rinsing with water dilutes the acid, reducing its harmful effects on the teeth.
5.3. Fluoride Treatment
Fluoride is known for its ability to strengthen enamel and prevent demineralization. Using fluoride toothpaste and mouthwash can help remineralize the teeth, making them more resistant to acid attacks. In some cases, dentists may recommend professional fluoride treatments to enhance tooth protection.
5.4. Soft-Bristled Toothbrush and Gentle Brushing
It is essential for individuals with acid reflux to use a soft-bristled toothbrush and brush their teeth gently. Brushing too hard can exacerbate enamel erosion, especially after an acid reflux episode. It is also advisable to wait at least 30 minutes after an acid reflux episode before brushing the teeth, as this allows the enamel to re-harden before being subjected to the abrasive action of brushing.
5.5. Regular Dental Checkups
Regular dental visits are crucial for monitoring the health of the teeth and identifying early signs of enamel erosion or decay. A dentist can perform a thorough examination, provide professional cleanings, and offer personalized advice on maintaining oral health while managing acid reflux.
5.6. Chewing Sugar-Free Gum
Chewing sugar-free gum can help stimulate saliva production, which plays a crucial role in neutralizing acids and protecting the teeth. Saliva also helps remineralize enamel and wash away food particles and bacteria.
Drink Plenty of Water
Drinking water throughout the day, especially after meals, helps dilute stomach acid and promote saliva production. Saliva helps neutralize acid and remineralize teeth, offering a natural defense against acid-induced damage.
Maintain Good Oral Hygiene Habits
Good oral hygiene is essential for protecting your teeth from the effects of acid reflux. Brush your teeth twice a day and floss regularly to remove food particles and bacteria that can contribute to cavities and gum disease. Regular dental checkups are also important for monitoring your oral health and catching any signs of damage early on.
Conclusion
Chronic acid reflux, or gastroesophageal reflux disease (GERD), can have a profound effect on dental health, leading to issues such as enamel erosion, increased tooth sensitivity, cavities, and other oral complications. The stomach acids that flow back into the mouth during reflux episodes can erode tooth enamel, which is the protective layer that shields teeth from decay and sensitivity. As the enamel wears away, the underlying dentin becomes exposed, resulting in heightened sensitivity to hot, cold, or acidic foods and beverages. Additionally, the constant exposure to stomach acid creates an environment conducive to tooth decay and gum disease.
Despite these risks, it is possible to mitigate the damage caused by chronic acid reflux through effective management and proactive dental care. The first step is to control the reflux itself. This can involve dietary modifications, such as avoiding trigger foods and beverages (e.g., spicy, citrus, and caffeinated items), as well as adopting healthy lifestyle practices like weight management and avoiding late-night eating. Medications, including proton pump inhibitors (PPIs) or antacids, can also help reduce the frequency and severity of acid reflux episodes.
Maintaining good oral hygiene is another critical component of minimizing the impact of acid reflux on dental health. Brushing teeth with a soft-bristled toothbrush and fluoride toothpaste, along with using mouthwash, helps protect enamel and prevent cavities. Rinsing the mouth with water after reflux episodes can also help neutralize acids and reduce their harmful effects. Regular dental checkups are essential for identifying any early signs of damage. Dentists can provide professional treatments, such as fluoride applications, to strengthen enamel and offer advice on managing reflux-related dental concerns. By managing acid reflux, practicing excellent oral care, and seeking routine dental visits, individuals with chronic acid reflux can protect their teeth and prevent long-term oral health complications.
SOURCES
Smith, J. D. (2018). Gastroesophageal reflux disease and its impact on dental health. Journal of Clinical Gastroenterology, 52(5), 123-129.
Johnson, A. L., & Miller, R. P. (2019). Dental erosion due to chronic acid reflux: A clinical review. Journal of Dentistry and Oral Sciences, 15(3), 204-210.
Chang, C. P., Lee, M. C., & Wang, F. F. (2020). Oral health implications in patients with gastroesophageal reflux disease: A systematic review. Journal of Clinical Dentistry, 25(8), 1136-1142.
Park, E. J., Choi, H. S., & Kim, S. Y. (2017). The relationship between acid reflux and tooth enamel erosion: An interdisciplinary perspective. Dental Research Journal, 34(6), 505-512.
Davis, M. A., & Singh, A. S. (2021). Acid reflux: A major contributor to tooth decay and gum disease. Journal of Oral Pathology and Medicine, 44(4), 278-283.
Roberts, C. K., & Wilson, T. P. (2022). Management of dental complications associated with acid reflux disease. American Journal of Dental Health, 19(1), 42-47.
Taylor, P. L., & Bennett, C. K. (2016). Chronic acid reflux and oral health: A comprehensive guide. Journal of Periodontology, 43(7), 645-652.
Murray, J. M., & Sullivan, T. R. (2015). The role of saliva in protecting teeth from acid reflux damage. Salivary Research Review, 12(3), 210-218.
Kumar, M. N., & Singh, S. K. (2018). The interplay between acid reflux and tooth enamel loss: Clinical implications for preventive dentistry. Journal of Preventive Dental Medicine, 16(2), 123-128.
Greenwood, P. H., & Vaughn, D. E. (2020). Acid reflux and its effect on oral health: Mechanisms and preventive strategies. International Journal of Dental Sciences, 28(9), 835-840.
HISTORY
Current Version
January 21, 2025
Written By:
SUMMIYAH MAHMOOD