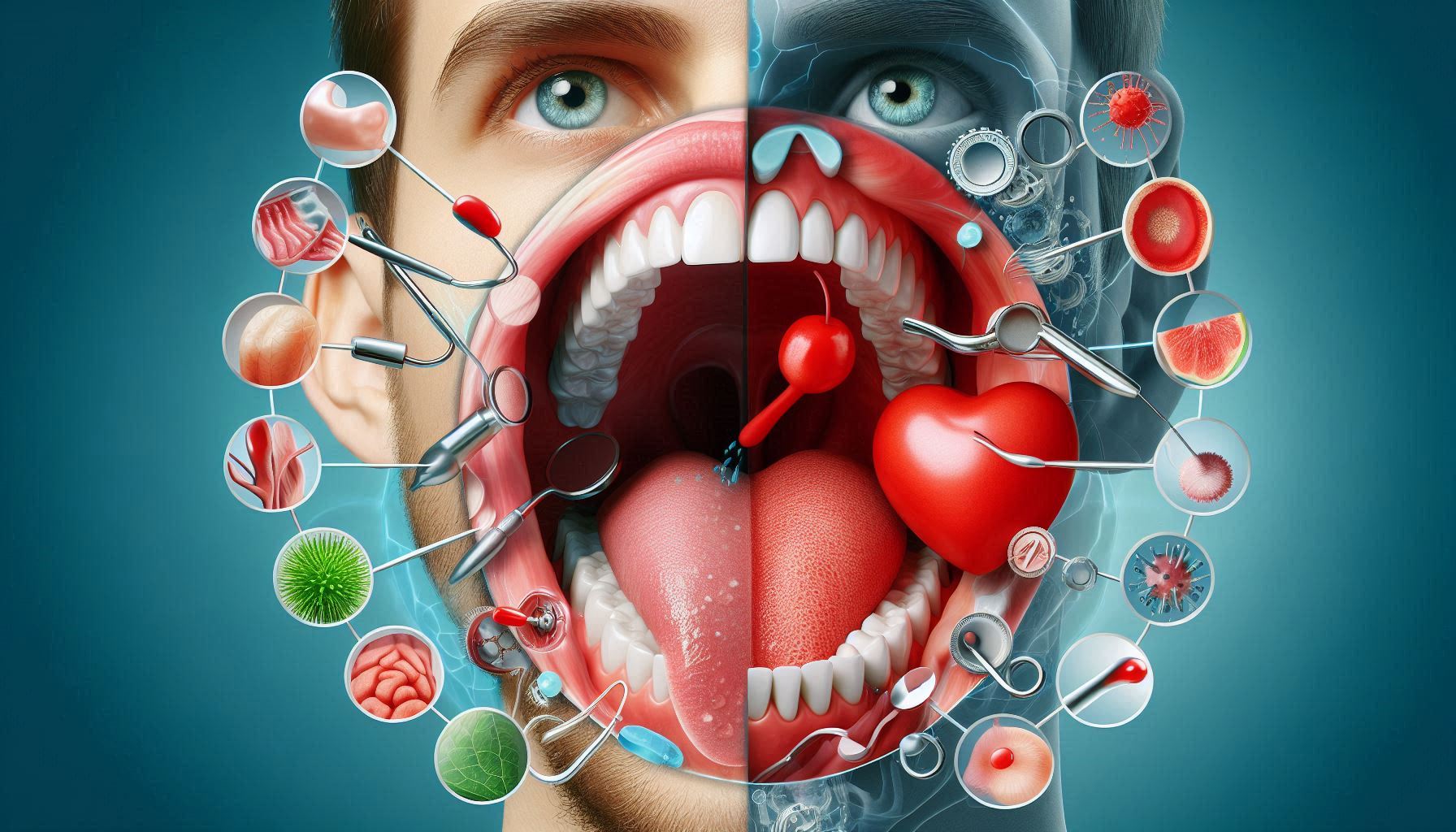
Your gums are not just a part of your mouth; they’re also crucial indicators of your overall health. The state of your gums can reveal important insights about your body, offering clues to conditions that extend well beyond dental health. A growing body of research is uncovering the hidden links between gum health and systemic conditions, which include heart disease, diabetes, respiratory issues, and even cognitive decline. The profound connection between oral care and chronic diseases highlights the importance of maintaining healthy gums for long-term well-being.
Though we often focus on our teeth when considering oral health, gums are just as vital. The gums serve not only as a protective barrier but also as an early warning system. Infected, inflamed, or receding gums could signal underlying health issues that, if left unaddressed, can have far-reaching effects. The intricate relationship between oral health and systemic conditions underscores the significance of routine dental care and proper hygiene in managing and preventing chronic diseases.
This guide aims to explore how gum health is linked to broader chronic health conditions, emphasizing the importance of regular oral care in both prevention and management of these illnesses.
Understanding Gum Disease in Detail
What is Gum Disease?
Gum disease, or periodontal disease, is an infection of the tissues that support the teeth, including the gums, ligaments, and bones. It begins when plaque, a sticky film of bacteria, accumulates on the teeth. If plaque is not removed regularly by brushing and flossing, it hardens into tartar, which is much harder to remove without professional cleaning.
At the initial stage, gum disease is referred to as gingivitis. Gingivitis is characterized by red, swollen, and bleeding gums, especially when brushing or flossing. This early stage is usually reversible with proper oral care. However, if left untreated, gingivitis can progress into periodontitis, a more severe form of gum disease. Periodontitis can result in the loss of tooth-supporting bone, receding gums, and in extreme cases, tooth loss.
The Causes of Gum Disease
Gum disease is primarily caused by the accumulation of plaque, which contains bacteria. However, several factors can contribute to the development and progression of gum disease, including:
- Poor Oral Hygiene: Inadequate brushing and flossing allow plaque to build up, leading to gum disease.
- Smoking or Chewing Tobacco: Tobacco products can impair gum health by reducing blood flow to the gums, making them more vulnerable to infection.
- Genetics: Some people may be genetically predisposed to gum disease.
- Medications: Certain medications, such as those that reduce saliva production, can increase the risk of gum disease.
- Other Health Conditions: Diseases like diabetes, HIV/AIDS, and certain autoimmune disorders can affect the immune system, making it harder to fight off gum infections.
- Hormonal Changes: Pregnancy, menstruation, and menopause can increase susceptibility to gum disease due to hormonal shifts.
- Poor Nutrition: A lack of nutrients, especially vitamin C, can weaken gum tissue, leading to gum problems.
How Gum Disease Progresses
Gum disease typically progresses in stages, starting from gingivitis to periodontitis, and eventually to advanced periodontitis if left untreated. Understanding the stages of gum disease helps in identifying early warning signs:
- Gingivitis: This early stage of gum disease is marked by inflamed, red, and bleeding gums. Gingivitis is usually painless and may go unnoticed unless the gums bleed during brushing or flossing.
- Mild Periodontitis: If gingivitis is not treated, it can progress to mild periodontitis, where the inflammation spreads deeper into the gums, affecting the supporting ligaments. Mild periodontitis may lead to the formation of pockets between the teeth and gums.
- Moderate Periodontitis: At this stage, the infection spreads deeper into the supporting bone and tissues, leading to more severe gum recession, bone loss, and tooth mobility. Pockets around the teeth become larger, trapping food particles and bacteria.
- Advanced Periodontitis: In this final stage, severe damage has occurred to the gum tissue and supporting bone. Teeth may become loose, and tooth loss is common. Treatment at this stage often involves surgical intervention, and in some cases, tooth extraction.
Symptoms of Gum Disease
The symptoms of gum disease can vary depending on the stage, but common signs include:
- Red, swollen, or bleeding gums
- Persistent bad breath (halitosis)
- Receding gums
- Sensitive teeth
- Loose or shifting teeth
- Painful chewing
- Pus between teeth and gums
- A change in bite or the fit of dentures
It’s important to note that gum disease may not always cause noticeable pain, especially in its early stages. Therefore, regular dental check-ups are critical in identifying and treating gum disease before it progresses.
The Oral-Systemic Health Connection
The Mouth as a Gateway to the Body
The mouth is often referred to as a “gateway” to the body because it can provide insight into overall health. The presence of bacteria in the mouth can spread to other areas of the body, leading to chronic inflammation, which plays a significant role in various systemic diseases. This connection between oral health and systemic health is known as the oral-systemic link.
Research has shown that the bacteria responsible for gum disease can enter the bloodstream through the gums, especially when the gums are inflamed or bleeding. Once in the bloodstream, these bacteria can travel to other organs and tissues, potentially causing widespread inflammation and contributing to the development or worsening of chronic health conditions.
The Role of Inflammation
Inflammation is a key player in the development of many chronic diseases, and gum disease is a significant source of chronic inflammation. When the gums are infected, the body’s immune response triggers the release of inflammatory markers, which can travel throughout the body and cause systemic effects. Chronic inflammation can lead to the progression of diseases such as cardiovascular disease, diabetes, respiratory conditions, and even neurodegenerative disorders.
Gum Disease and Cardiovascular Health
The Link Between Gum Disease and Heart Disease
Numerous studies have found a connection between gum disease and cardiovascular disease, particularly heart disease. The exact mechanism behind this relationship is still being studied, but several theories have emerged:
- Bacterial Invasion: As mentioned earlier, bacteria from infected gums can enter the bloodstream. These bacteria may attach to the walls of blood vessels, leading to the formation of plaques and promoting atherosclerosis (narrowing and hardening of the arteries). This can increase the risk of heart attack, stroke, and other cardiovascular problems.
- Inflammatory Response: Chronic inflammation from gum disease can contribute to systemic inflammation, which is a known risk factor for heart disease. Inflammation can damage blood vessel walls, increasing the likelihood of plaque buildup and the formation of blood clots.
- Endothelial Dysfunction: Some studies suggest that the bacteria associated with gum disease can contribute to endothelial dysfunction (impaired function of the blood vessel lining), a key factor in the development of cardiovascular disease.
Studies and Evidence
A 2019 study published in the Journal of Clinical Periodontology found that individuals with gum disease were more likely to experience a heart attack or stroke than those with healthy gums. Other studies have shown that treating gum disease can have a positive effect on cardiovascular health, suggesting that proper oral care can reduce the risk of heart-related issues.
How to Protect Your Heart by Caring for Your Gums
To reduce the risk of cardiovascular disease, it’s important to maintain good oral hygiene. Brushing twice a day, flossing daily, and visiting the dentist regularly for professional cleanings are all essential practices. Additionally, adopting heart-healthy habits such as eating a balanced diet, exercising regularly, and avoiding smoking can further reduce the risk of both gum disease and heart disease.
Diabetes and Gum Disease: A Bidirectional Relationship
How Gum Disease Affects Diabetes
There is a strong bidirectional relationship between gum disease and diabetes. People with diabetes are more susceptible to gum disease because high blood sugar levels can impair the body’s ability to fight infections. Elevated blood sugar also leads to the thickening of blood vessels, which can restrict blood flow to the gums, making them more vulnerable to bacterial infection.
Moreover, individuals with poorly controlled diabetes may experience delayed wound healing, making it harder for their bodies to repair the damage caused by gum disease.
How Gum Disease Affects Blood Sugar Control
On the flip side, gum disease can make it more difficult to control blood sugar levels. The inflammation triggered by gum disease can interfere with the body’s ability to use insulin effectively, potentially leading to higher blood sugar levels. Studies have shown that treating gum disease can improve blood sugar control in individuals with diabetes, indicating that good oral health can positively affect diabetes management.
Managing Gum Disease in Diabetic Patients
For individuals with diabetes, it is especially important to monitor oral health regularly. Regular dental check-ups, professional cleanings, and good home care practices (brushing and flossing) are crucial in preventing and managing gum disease. Additionally, maintaining blood sugar control through diet, exercise, and medication is essential in preventing the onset or progression of gum disease.
Respiratory Diseases and Gum Health
How Oral Bacteria Contribute to Respiratory Infections
The link between oral health and respiratory diseases is often overlooked. Oral bacteria can be aspirated (inhaled) into the lungs, where they can cause respiratory infections such as pneumonia. This is particularly concerning for individuals with weakened immune systems, those who are elderly, or individuals with pre-existing respiratory conditions such as chronic obstructive pulmonary disease (COPD).
Research has shown that people with gum disease are at a higher risk of developing respiratory diseases, including pneumonia, bronchitis, and even exacerbations of COPD. In these cases, treating gum disease has been shown to reduce the frequency and severity of respiratory infections.
The Role of Oral Hygiene in Preventing Respiratory Infections
Good oral hygiene plays a key role in reducing the risk of respiratory infections. Brushing, flossing, and professional cleanings help reduce the bacteria in the mouth, minimizing the chances of these bacteria being aspirated into the lungs. Individuals with respiratory conditions should be especially diligent about their oral care to prevent complications.
Gum Disease and Pregnancy Complications
The Risks of Gum Disease During Pregnancy
Pregnancy can affect gum health due to hormonal changes that increase susceptibility to gum disease. Pregnant women with gum disease are at an increased risk of complications, including preterm birth, low birth weight, and gestational diabetes. The inflammation caused by gum disease can trigger the release of chemicals that may interfere with fetal development.
Some studies have found that women with untreated gum disease during pregnancy are more likely to deliver prematurely or have a baby with low birth weight.
Preventing Gum Disease During Pregnancy
To reduce the risk of pregnancy complications related to gum disease, it’s important to maintain good oral hygiene during pregnancy. Regular dental visits are essential for monitoring gum health. If gum disease is detected, prompt treatment can help prevent complications.
Alzheimer’s Disease and Cognitive Decline
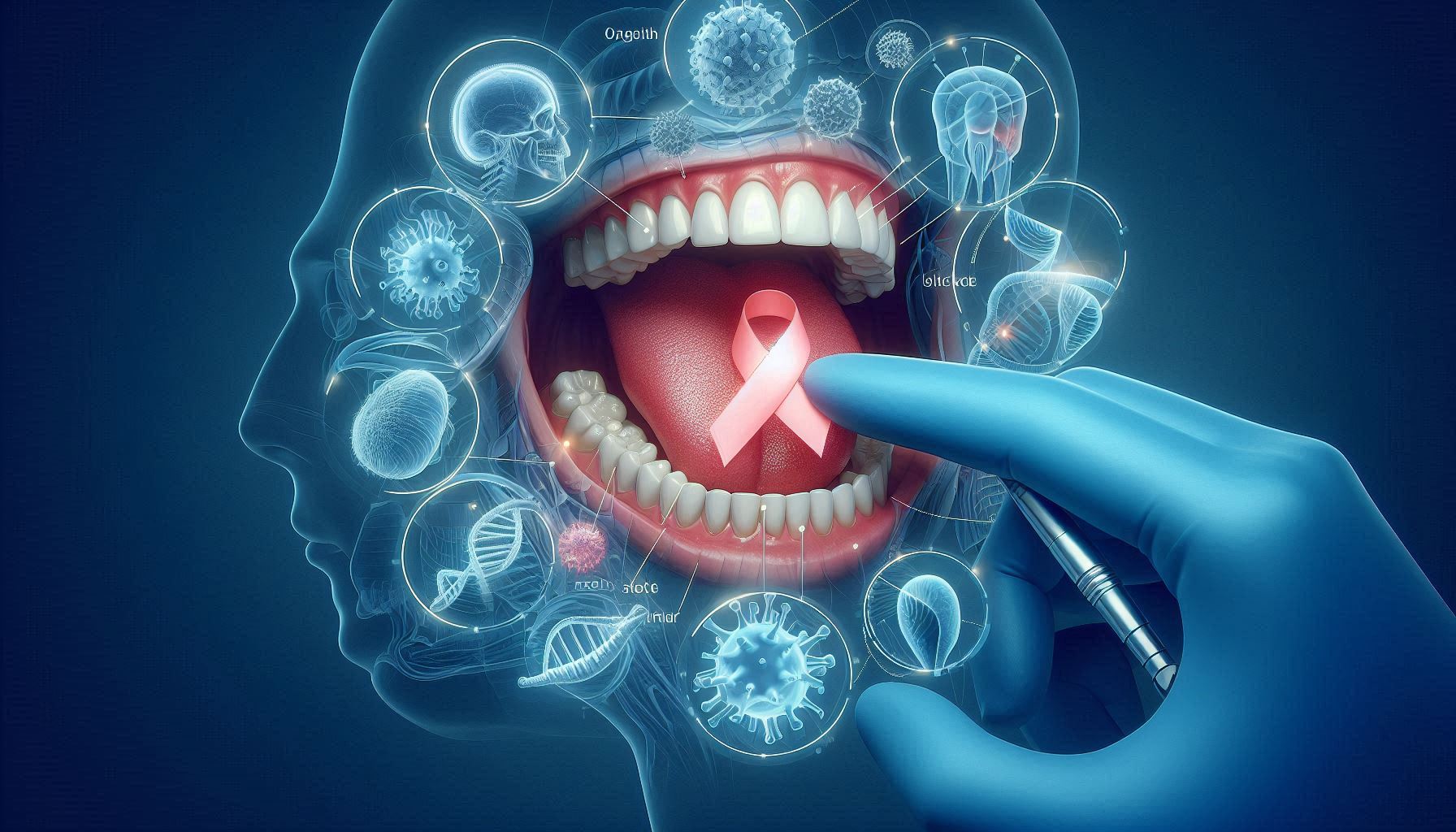
The Connection Between Gum Disease and Alzheimer’s Disease
Recent studies have suggested a potential link between gum disease and Alzheimer’s disease. Researchers believe that bacteria from the mouth, particularly Porphyromonas gingivalis, a bacterium associated with gum disease, may travel through the bloodstream and reach the brain. There, the bacteria may trigger an inflammatory response, which could contribute to the development of Alzheimer’s or accelerate its progression.
While this research is still in its early stages, the potential connection between gum disease and Alzheimer’s disease has prompted further investigation into how oral health might influence brain health.
How Oral Health Might Impact Cognitive Decline
By maintaining good oral hygiene and treating gum disease early, individuals may reduce their risk of developing cognitive decline or dementia later in life. Although more research is needed, current studies suggest that oral health plays a significant role in maintaining cognitive function, particularly in older adults.
Conclusion
The health of your gums is much more than a cosmetic concern; it is a crucial indicator of your overall health. Gum disease is linked to a range of chronic conditions, including heart disease, diabetes, respiratory infections, pregnancy complications, and even cognitive decline. Regular dental visits, good oral hygiene practices, and a healthy lifestyle are essential for preventing and managing gum disease, which in turn can reduce the risk of these chronic conditions.
By taking care of your gums, you are not only ensuring a healthy smile but also protecting your long-term health. The mouth is the gateway to the body, and the state of your gums can reveal critical information about your well-being. Don’t wait for a toothache or gum bleeding to seek help—take proactive steps to maintain your oral health and improve your overall quality of life.
SOURCES
Al-Zahrani, M. S., 2011. The relationship between periodontal disease and cardiovascular disease. Journal of Periodontal Research, 46(6), 607-615.
Beck, J. D., 2014. The effect of periodontal disease on systemic diseases: A review of the literature. Journal of Periodontology, 85(7), 887-896.
Bergström, J., 2000. Periodontal disease and systemic conditions: A literature review. Journal of Clinical Periodontology, 27(1), 1-10.
Borrell, L. N., 2012. Associations between oral hygiene and systemic diseases. Journal of Clinical Periodontology, 39(10), 933-944.
Chaves, R. S., 2014. Effect of periodontal therapy on blood sugar levels in diabetic patients. Journal of Diabetes and Its Complications, 28(3), 356-361.
D’Aiuto, F., 2004. Periodontal disease and cardiovascular disease: A review. Journal of Periodontology, 75(3), 496-505.
Desvarieux, M., 2013. Periodontal disease and risk of coronary heart disease: The Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation, 107(3), 353-357.
Genco, R. J., 2009. Host responses in periodontal diseases: Current concepts. Journal of Periodontology, 80(4), 552-561.
Hyman, D., 2006. Diabetes and oral health. American Family Physician, 74(4), 623-628.
Kaur, S., 2020. Periodontitis and its connection to systemic diseases: A systematic review. Journal of Clinical and Diagnostic Research, 14(6), ZE01-ZE05.
Loos, B. G., 2017. Systemic effects of periodontitis. Journal of Clinical Periodontology, 44(3), S45-S59.
Mattila, K. J., 1995. Periodontal disease and risk of acute myocardial infarction: A population-based study. American Journal of Epidemiology, 142(8), 741-746.
Sato, T. & Miyazaki, H., 2007. Periodontal disease and its potential connection to respiratory diseases. Journal of Periodontal Research, 42(4), 390-395.
Socransky, S. S., 2003. Microbial complexes in subgingival plaque. Journal of Clinical Periodontology, 30(6), 74-81.
Taba, M. & Huang, Y., 2013. The role of periodontal disease in systemic health. Journal of Periodontology, 84(9), 1265-1277.
Taylor, G. W., 2001. Bidirectional interrelationships between diabetes and periodontal diseases: An epidemiologic perspective. Annals of Periodontology, 6(1), 99-112.
Tonetti, M. S., 2013. Treatment of periodontitis and systemic disease: Evidence and implications for practice. Periodontology 2000, 62(1), 43-67.
Van Dyke, T. E., 2014. The role of inflammation in periodontal disease: A review of the mechanisms. Journal of Periodontology, 85(6), 684-693.
Wimmer, D. W., 2017. The impact of periodontal disease on respiratory diseases. Journal of Respiratory Medicine, 111(2), 239-245.
HISTORY
Current Version
January 14, 2025
Written By:
SUMMIYAH MAHMOOD