Introduction
Gum disease, also known as periodontal disease, is a common dental condition that affects the gums and the structures supporting the teeth. If left untreated, it can lead to tooth loss and may contribute to other health problems, including cardiovascular disease, diabetes, and respiratory issues. Gum disease typically develops as a result of poor oral hygiene, which allows plaque—a sticky film of bacteria—to form on the teeth and gums. If not removed, plaque can turn into tartar (calculus), leading to inflammation of the gums, known as gingivitis.
In this guide, we will discuss the early symptoms of gum disease, the preventive measures you can take, and the treatment options available for managing and reversing the condition.
Understanding Gum Disease: The Basics
Gum disease is a chronic infection that begins when bacteria accumulate in the pockets of the gums around the teeth. The infection can affect the gums (gingivitis) and, if left untreated, progress to the bone and tissue supporting the teeth (periodontitis).
The Two Main Stages of Gum Disease
- Gingivitis: Gingivitis is the earliest stage of gum disease and is usually reversible with proper oral hygiene. It occurs when plaque builds up on the teeth and irritates the gum tissue, causing redness, swelling, and bleeding, especially during brushing and flossing. The hallmark symptom of gingivitis is bleeding gums.
- Periodontitis: If gingivitis is not treated, it can advance to periodontitis. This stage involves more severe inflammation and can lead to the destruction of gum tissue and bone. Periodontitis may cause the gums to recede, pockets to form between the teeth and gums, and in severe cases, tooth mobility or loss.
The Anatomy of Gum Disease
Before discussing symptoms, prevention, and treatment, it is helpful to understand the biological processes that underlie gum disease. Understanding these processes allows for a better grasp of why gum disease develops and how treatment options work to reverse or manage the condition.
The Structure of Healthy Gums
Healthy gums play a crucial role in oral health. They provide a barrier to bacteria and help protect the underlying bone and tooth structure. The main components of healthy gums include:
- Gingiva: The gingiva is the soft tissue that surrounds the teeth and covers the jawbone. It is typically pink and firm, tightly hugging the tooth. The gingiva is composed of several layers that protect the underlying structures from infection.
- Gingival Sulcus: This is the small space between the gum and the tooth. In healthy individuals, the gingival sulcus measures 1-3 millimeters in depth. If the sulcus deepens, it can lead to the formation of pockets, which are a sign of gum disease.
- Periodontal Ligament: This structure attaches the teeth to the jawbone and supports tooth movement.
- Alveolar Bone: The alveolar bone forms the sockets that hold the roots of the teeth. The health of this bone is critical in preventing tooth loss.
The Role of Plaque in Gum Disease
The development of gum disease begins with the accumulation of plaque, a sticky film of bacteria that forms on the teeth. Plaque is made up of food particles, bacteria, and saliva, and it builds up more rapidly on the teeth’s surfaces, especially along the gumline.
If plaque is not removed by regular brushing and flossing, it turns into tartar, or calculus, a hardened form of plaque. Tartar can only be removed by a dental professional. Tartar provides a breeding ground for bacteria, which can irritate the gums and lead to inflammation.
The Bacteria Behind Gum Disease
The bacteria responsible for gum disease primarily include Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola. These bacteria feed on sugars and food particles in the mouth and produce toxins that damage the gum tissues, leading to the progression of gingivitis and, eventually, periodontitis.
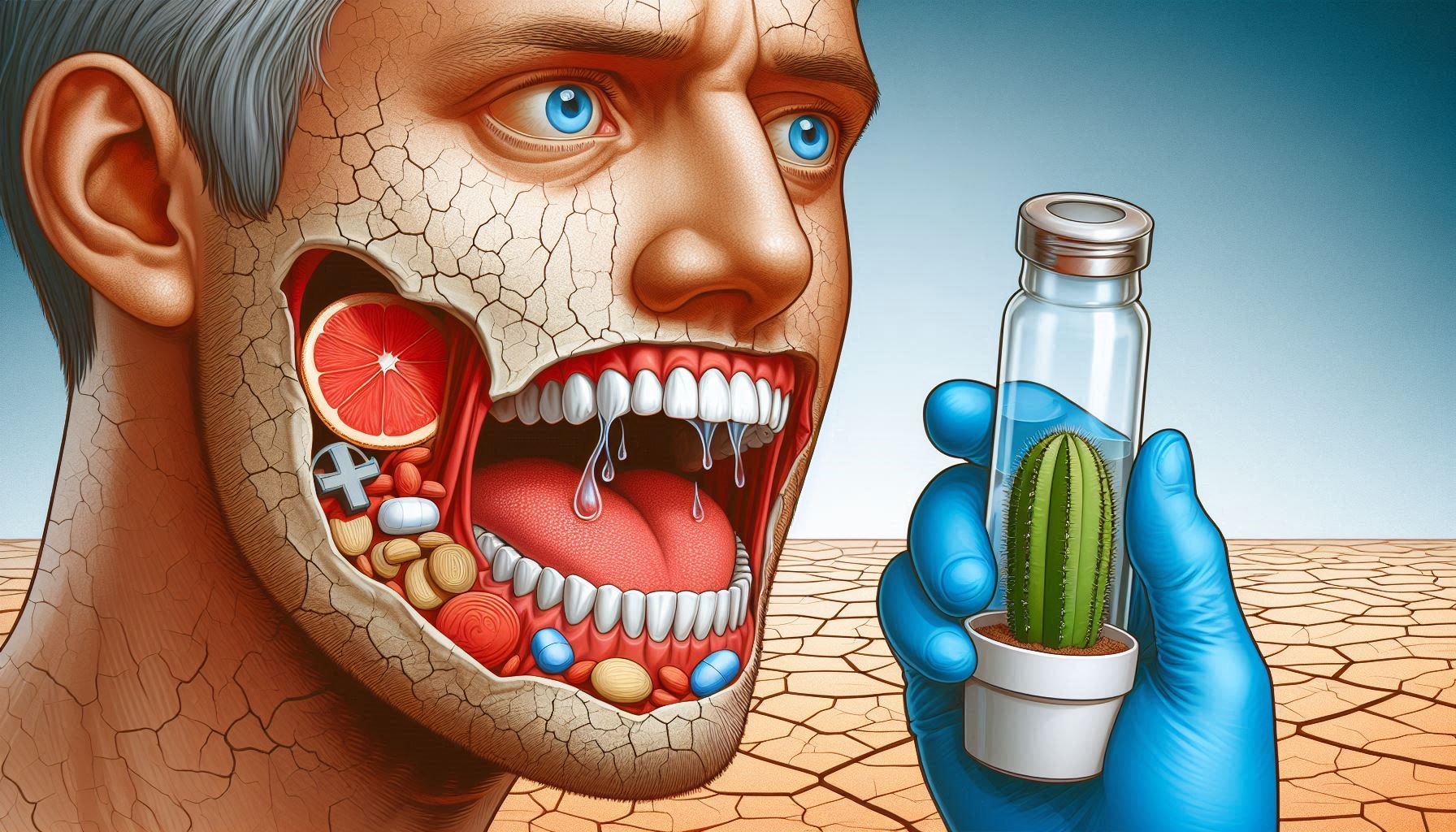
The Early Symptoms of Gum Disease
Recognizing the early symptoms of gum disease is crucial for preventing its progression. Many individuals may overlook the initial signs, as they may not cause significant pain. However, the following symptoms are key indicators that should prompt you to seek dental advice.
Red or Swollen Gums
Healthy gums should be a pale pink color. Red or swollen gums are early signs of inflammation, which is caused by bacterial irritation. The increased blood flow to the affected area causes the gums to become red, swollen, and tender. At this stage, the condition is usually classified as gingivitis and is still reversible.
Bleeding Gums
Bleeding gums, particularly when brushing or flossing, is one of the most common signs of gum disease. This is because the bacteria in plaque cause irritation and inflammation in the gum tissues. As a result, the blood vessels in the gums become more fragile, and even slight pressure from a toothbrush or floss can cause bleeding. If you experience bleeding gums consistently, it is an indication that the plaque buildup is severe enough to cause damage to the gums.
Persistent Bad Breath (Halitosis)
One of the first signs of gum disease that people notice is bad breath, which can be persistent even after brushing and using mouthwash. This occurs because bacteria in the mouth release sulfur compounds, which produce an unpleasant odor. As gum disease progresses, the bad breath may worsen, and you may notice a bad taste in your mouth as well.
Gum Recession
Gum recession occurs when the gum tissue pulls back from the teeth, exposing more of the tooth or even the tooth’s root. This is often a sign of advanced gum disease. As the infection progresses, the supporting tissues around the teeth begin to break down, causing the gums to recede. Gum recession is typically associated with periodontitis and can lead to sensitivity and the appearance of longer teeth.
Pocket Formation Between Teeth and Gums
As gum disease progresses, pockets or gaps form between the teeth and gums, which can trap food particles and bacteria. The formation of these pockets indicates the progression of gingivitis to periodontitis, where deeper tissues are affected. If left untreated, the pockets can become deeper and more prone to infection, leading to further damage to the supporting structures of the teeth.
Tooth Sensitivity
Gum disease can lead to the exposure of the tooth’s roots, which are not covered by enamel. When the roots become exposed, they are more sensitive to temperature changes, such as hot or cold food and beverages. If you experience sensitivity in your teeth, particularly in areas where the gums have receded, this may be a sign of gum disease.
How to Prevent Gum Disease: A Comprehensive Guide
While gum disease is common, it is largely preventable with good oral hygiene practices and lifestyle changes. In this section, we will cover the steps you can take to prevent gum disease and maintain healthy gums for life.
Brush Your Teeth Properly
Brushing your teeth is the first line of defense against plaque buildup. Proper brushing removes plaque from the surfaces of your teeth and gums, preventing it from hardening into tartar. The following tips will help you brush effectively:
- Use a Soft-Bristled Toothbrush: A toothbrush with soft bristles is gentler on your gums and tooth enamel. Hard bristles can cause gum irritation and enamel erosion, which can contribute to gum disease.
- Brush Twice a Day: Brush your teeth at least twice a day—once in the morning and once before bed. Make sure to brush for at least two minutes each time, ensuring that you cover all surfaces of your teeth and gums.
- Use Fluoride Toothpaste: Fluoride toothpaste helps to strengthen the enamel and fight against tooth decay. It also helps prevent plaque buildup, which can lead to gum disease.
- Use Proper Technique: Hold the toothbrush at a 45-degree angle to your gums and use gentle, circular motions to clean the teeth. Avoid brushing with harsh back-and-forth motions that can irritate the gums.
Floss Daily
Flossing is an essential part of maintaining good oral hygiene, as it removes plaque and food particles from between your teeth and along the gumline—areas that your toothbrush may not reach. Daily flossing reduces the buildup of plaque and prevents gum disease from developing in these hard-to-reach areas.
- Be Gentle: When flossing, be gentle and avoid snapping the floss between your teeth, as this can cause gum injury. Instead, gently slide the floss between your teeth and curve it around each tooth to clean the surface.
Rinse with an Antimicrobial Mouthwash
Mouthwash can help reduce bacteria in the mouth, promote fresh breath, and provide an extra layer of protection against gum disease. Look for an antimicrobial mouthwash that contains ingredients like chlorhexidine or essential oils (e.g., eucalyptol and thymol) to fight plaque and gingivitis-causing bacteria.
Regular Dental Checkups
One of the best ways to prevent gum disease is by scheduling regular dental checkups. Professional cleanings are essential because they remove plaque and tartar that may have built up on your teeth. During these visits, your dentist or hygienist will also examine your gums for any signs of infection, swelling, or recession, allowing for early detection and treatment of gum disease.
Quit Smoking and Tobacco Use
Smoking and tobacco use are major risk factors for gum disease. Tobacco reduces blood flow to the gums, making it more difficult for them to heal. Smokers are also more likely to have plaque buildup and gum infections. Quitting smoking significantly improves the health of your gums and reduces the risk of gum disease.
Maintain a Healthy Diet
A balanced diet rich in vitamins and minerals supports strong gums and teeth. Specifically, vitamin C is essential for gum health because it helps prevent inflammation and bleeding. Foods rich in vitamin C include citrus fruits, strawberries, bell peppers, and leafy greens. In addition to vitamin C, calcium is important for strengthening the teeth and bones. Dairy products, leafy greens, and fortified non-dairy alternatives are excellent sources of calcium.
Stay Hydrated
Drinking plenty of water is essential for maintaining good oral health. Water helps rinse away food particles and bacteria from the mouth, reducing the likelihood of plaque buildup. It also promotes healthy saliva flow, which plays an important role in neutralizing acids and fighting oral bacteria.
Treatment Options for Gum Disease
Non-Surgical Treatment
For early stages of gum disease (gingivitis), treatment is often non-invasive and can be performed by a dentist or dental hygienist:
- Scaling and Polishing (Professional Cleaning): Scaling is the process of removing plaque and tartar from the teeth, while polishing helps smooth the tooth surfaces. Scaling and polishing are usually done during routine dental cleanings and can effectively treat early-stage gum disease.
- Antibiotics: In some cases, antibiotics may be prescribed to help control bacterial infection. These may be topical (applied directly to the gums) or oral antibiotics. Topical antibiotics are often used after scaling to ensure that bacteria are eliminated from the gum pockets.
Surgical Treatment
If gum disease progresses to periodontitis and non-surgical treatments are ineffective, surgical options may be necessary:
- Flap Surgery: During flap surgery, the gums are lifted away from the teeth, allowing the dentist to access and clean the roots and underlying bone. Afterward, the gums are sutured back in place.
- Bone and Tissue Grafts: If the bone or tissue surrounding the teeth has been severely damaged by periodontitis, bone grafts or tissue grafts may be used to regenerate the lost tissue. These grafts can help stabilize the teeth and promote the healing of the gums.
If you’ve developed gum disease, early treatment can help manage the condition and prevent further damage. The type of treatment will depend on the severity of the gum disease, whether it is gingivitis or periodontitis.
Treatment for Gingivitis:
- Improved Oral Hygiene: The primary treatment for gingivitis involves improved oral hygiene practices. By brushing and flossing more effectively, you can eliminate plaque buildup and reduce inflammation in the gums. A dentist or dental hygienist can provide guidance on proper brushing and flossing techniques.
- Professional Cleaning (Scaling and Polishing): During a dental visit, the dentist or hygienist will perform a professional cleaning to remove plaque and tartar from the teeth and below the gumline. This procedure helps to reverse gingivitis by eliminating the sources of bacterial buildup.
Treatment for Periodontitis:
If gingivitis has progressed to periodontitis, more intensive treatment may be necessary to address the deeper infection and restore gum health.
- Scaling and Root Planing: Scaling and root planing is a non-surgical procedure in which the dentist or hygienist removes tartar from the teeth and smooths the roots to promote gum reattachment. This procedure is often done under local anesthesia and is effective in treating moderate periodontitis.
- Antibiotics: In some cases, your dentist may prescribe topical or oral antibiotics to help control bacterial infections. Antibiotics may be used after scaling and root planing or in conjunction with other treatments to help reduce inflammation and infection.
- Surgical Treatments: If periodontitis is severe and non-surgical treatments are not effective, surgery may be necessary. Surgical options include:
- Flap Surgery: The dentist makes incisions in the gum tissue to lift the gums and remove deep-seated tartar. The gums are then sutured back in place.
- Bone and Tissue Grafts: If the bone or tissue supporting the teeth has been destroyed, grafts may be used to encourage new growth and restore the gum structure.
- Laser Therapy: Laser treatment is a minimally invasive option for treating periodontitis. The laser is used to remove infected tissue and bacteria from the gums while stimulating the regeneration of healthy tissue.
Conclusion
Gum disease is a prevalent yet preventable condition that can have significant consequences if left untreated. Early detection and treatment are key to managing gum disease and maintaining good oral health. By practicing proper oral hygiene, visiting the dentist regularly, and making healthy lifestyle choices, you can significantly reduce your risk of developing gum disease and enjoy a lifetime of healthy teeth and gums. Remember, if you notice any early signs of gum disease, such as bleeding gums or bad breath, it’s important to seek treatment promptly. The earlier the intervention, the easier it is to reverse the condition and protect your teeth for years to come.
SOURCES
Albandar, J. M. (2002). Global epidemiology of periodontal diseases: An overview. Periodontology 2000, 29(1), 7-16.
Becker, W., & Greenstein, G. (2018). The role of periodontal therapy in the management of gum disease: A clinical perspective. Journal of Periodontology, 89(1), 4-12.
Brennan, M. T., & Reeve, C. M. (2006). The effect of smoking on periodontal disease: Mechanisms and management. Journal of Clinical Periodontology, 33(2), 127-134.
Cohen, D. W., & Rosen, R. L. (2016). Effectiveness of scaling and root planing in patients with periodontal disease: A meta-analysis. American Journal of Dentistry, 29(5), 293-297.
Eke, P. I., Dye, B. A., Wei, L., et al. (2015). Update on prevalence of periodontitis in the United States: NHANES 2009-2014. Journal of Periodontology, 86(5), 611-622.
Kornman, K. S., & Crane, A. (2008). Prevention and management of periodontal diseases: Current concepts. Periodontology 2000, 48(1), 19-32.
Löe, H. (1993). Periodontal disease: The sixth complication of diabetes mellitus. Diabetes Care, 16(1), 160-168.
Meyer, D. M., & Laskin, D. M. (2017). Clinical management of periodontal disease: A contemporary approach. Periodontology 2000, 75(1), 52-69.
Sanz, M., & Beighton, D. (2014). Diet and periodontal disease: A systematic review of the literature. Journal of Periodontal Research, 49(3), 244-250.
Tonetti, M. S., & Greenwell, H. (2017). Treatment of periodontitis: Systematic reviews and evidence-based guidelines. Journal of Clinical Periodontology, 44(Suppl 18), S150-S154.
Van der Weijden, F., & Hioe, K. P. L. (2005). A systematic review of the effectiveness of self-performed mechanical plaque control in the management of periodontal diseases. Journal of Clinical Periodontology, 32(3), 287-305.
Wang, H. L., & Rees, T. D. (2011). The effects of periodontal disease on systemic health: A review. Journal of Periodontal Research, 46(1), 1-12.
West, N. X., & Lalloo, R. (2012). Oral health and its association with systemic diseases. Periodontology 2000, 58(1), 24-32.
HISTORY
Current Version
February 5, 2025
Written By:
SUMMIYAH MAHMOOD