1. Introduction to Heart Disease and Toothache
The Complexity of Heart Disease
Heart disease is not just one condition but a broad spectrum of cardiovascular problems that affect millions worldwide. From coronary artery disease to arrhythmias, each type of heart disease presents its own unique set of symptoms, risk factors, and long-term effects. Coronary artery disease (CAD) is one of the leading causes of heart attacks, resulting from the narrowing of the arteries due to plaque buildup. Other forms of heart disease include valvular heart disease, congenital heart defects, and heart failure, among others. Each type can have varying symptoms, some of which may overlap with symptoms seen in other conditions like dental issues.
The symptoms of heart disease are often unmistakable—chest pain, shortness of breath, dizziness, and palpitations. However, there is a more subtle connection between heart disease and seemingly unrelated conditions like toothaches. The body’s various systems are interconnected in ways that can sometimes lead to a cascade of symptoms that may appear to be entirely unrelated.
What is a Toothache?
A toothache occurs when the sensitive tissue inside the tooth (the pulp) becomes irritated or inflamed. The pulp contains nerves and blood vessels, which can become painful when exposed to infection, pressure, or trauma. Toothaches are usually caused by cavities, gum disease, or abscesses—all of which allow bacteria to reach deeper tissues. The symptoms can range from sharp, stabbing pain to a dull, aching sensation that radiates to the jaw and surrounding areas.
Interestingly, pain in the teeth, gums, or jaw may not always be confined to dental problems. In some cases, pain in these areas can be a symptom of referred pain, a phenomenon where the brain perceives pain originating from a different part of the body. This is particularly significant when it comes to cardiovascular issues, where pain may radiate from the heart to other areas, including the teeth or jaw.
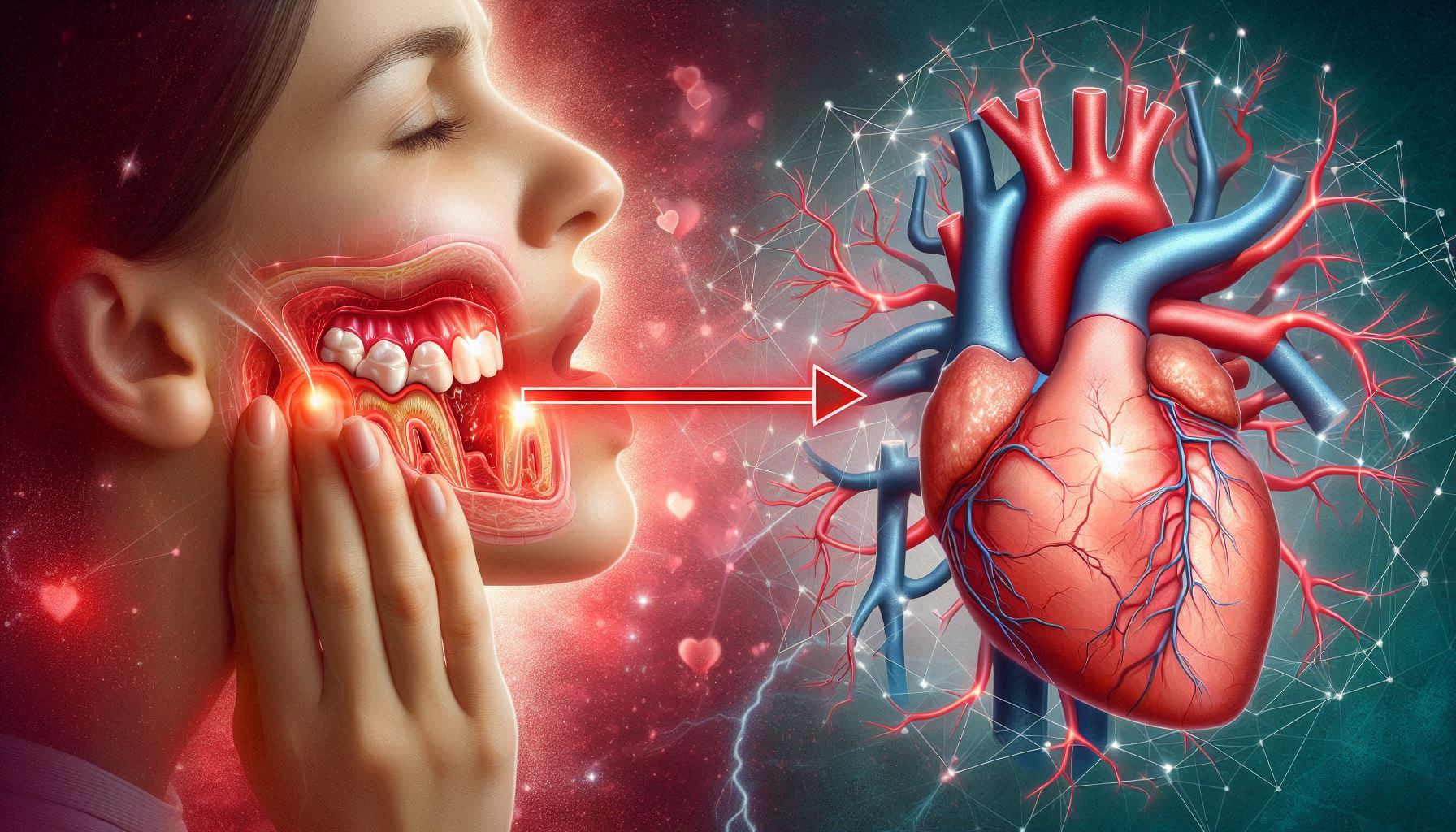
The Intersection of Dental and Heart Health
At first glance, heart disease and a toothache might seem unrelated, but the connection is more profound than we initially understand. The health of our gums and teeth may serve as an indicator of cardiovascular health, which is why dental health is often referred to as the “window to overall health.” Recent research suggests that periodontal disease—a severe form of gum disease—can increase the risk of heart disease. The bacteria associated with gum infections can enter the bloodstream and contribute to the formation of plaque in the arteries, which can lead to atherosclerosis and other cardiovascular problems.
The fact that inflammation in the gums can lead to systemic inflammation in the arteries is a key link in understanding how poor oral health could contribute to heart disease. Studies have shown that people with gum disease are more likely to have high blood pressure, high cholesterol, and higher levels of inflammation, all of which are significant risk factors for heart disease.
2. The Anatomy of the Heart and Mouth: How the Two Systems Are Connected
Heart Anatomy: Understanding the Circulatory System
The heart is a remarkable organ that serves as the central pump for blood circulation throughout the body. It has four chambers: the left and right atria (upper chambers) and the left and right ventricles (lower chambers). Blood flows through these chambers in a carefully coordinated cycle that ensures oxygen-rich blood is pumped throughout the body while carbon dioxide and waste products are carried away.
The left side of the heart pumps blood to the entire body, while the right side pumps blood to the lungs. Coronary arteries supply the heart muscle itself with oxygen-rich blood. When these arteries become blocked due to plaque buildup, the heart muscle may not receive enough oxygen, leading to a heart attack.
Oral Anatomy: The Mouth and Its Vital Functions
The mouth is composed of a complex structure, including teeth, gums, salivary glands, and the tongue, all of which play vital roles in digestion and overall health. The teeth are designed to chew and break down food, and their roots are embedded in the gums. These roots are rich in blood vessels and nerves, which makes them sensitive to pain when exposed to infection or injury.
The gums (or gingiva) surround the roots of the teeth and help protect the underlying bone and tissue. However, when the gums become inflamed (as in gingivitis), they may recede and leave the underlying tissue vulnerable to infection. Periodontal disease occurs when the infection spreads deeper into the tissues, potentially causing severe damage.
The Vascular Link Between Heart and Mouth
While it might seem like the heart and mouth are entirely separate systems, they are both part of the body’s vascular system, which is a network of blood vessels that carry oxygen, nutrients, and waste products throughout the body. Both the heart and mouth are deeply connected by the circulatory system, meaning that any inflammation or infection in the mouth has the potential to spread throughout the body.
The gingiva (gums) are connected to the blood vessels that transport oxygen and nutrients to the tissues. If the gums become infected or inflamed, bacteria can enter the bloodstream through the small blood vessels in the gums. These bacteria can travel to other parts of the body, including the arteries, where they may contribute to inflammation and plaque buildup, leading to atherosclerosis.
3. Understanding Toothaches: Causes, Symptoms, and Treatment
Causes of Toothaches
A toothache is typically caused by an infection, inflammation, or injury to the tooth. The most common causes of tooth pain include:
- Cavities: A cavity occurs when bacteria break down the enamel, leading to decay. This can expose the sensitive layers of the tooth, causing pain.
- Gum disease (Periodontitis): Infections in the gums can lead to pain in the teeth. As the infection spreads, it can cause the gums to recede, leading to tooth sensitivity.
- Tooth abscess: An infection in the root of the tooth or the surrounding tissues can lead to an abscess, which is an accumulation of pus that causes intense pain and swelling.
- Tooth fractures: A cracked or broken tooth can expose the pulp, leading to pain when chewing or drinking cold or hot beverages.
- Wisdom teeth: The eruption of wisdom teeth can cause discomfort, especially if they are impacted or misaligned.
Symptoms of Toothaches
Toothaches vary in intensity and duration. Common symptoms of a toothache include:
- Sharp, throbbing pain: Often caused by cavities or infections in the pulp of the tooth.
- Dull, aching pain: Can be a result of gum disease or an early-stage cavity.
- Pain when chewing or touching the tooth: A sign that the tooth is cracked or has an abscess.
- Sensitivity to temperature: Some toothaches are triggered by exposure to hot or cold food or drinks.
- Swelling around the tooth: This can be a sign of an infection that has spread to the gums or jawbone.
Treatment for Toothaches
Treatment for a toothache depends on the underlying cause:
- Fillings: For cavities, dentists often use fillings to restore the damaged tooth structure.
- Root canal therapy: For tooth abscesses or infected pulp, a root canal may be necessary to remove the infected tissue and seal the tooth.
- Antibiotics: In cases of infection, antibiotics may be prescribed to control bacteria.
- Gum disease treatment: Scaling and root planing can remove plaque and tartar from below the gum line, addressing the source of the infection.
- Tooth extraction: If a tooth is severely damaged or decayed, it may need to be removed to prevent the infection from spreading.
4. Heart Disease: More Than Just a “Heart Attack”
Types of Heart Disease
Heart disease encompasses various conditions, many of which are chronic and progressive. Some of the most common types include:
- Coronary Artery Disease (CAD): Caused by plaque buildup in the coronary arteries, leading to reduced blood flow to the heart.
- Heart Attacks (Myocardial Infarctions): Occurs when a blockage in the coronary arteries causes the heart muscle to be deprived of oxygen, leading to tissue death.
- Arrhythmias: Abnormal heart rhythms that can lead to ineffective pumping of the heart.
- Heart Failure: A condition in which the heart is unable to pump blood efficiently, leading to fluid buildup in the lungs and other parts of the body.
- Valvular Disease: Problems with one or more of the heart’s valves can lead to blood flow issues and increased strain on the heart.
Causes and Risk Factors for Heart Disease
The causes and risk factors for heart disease are numerous and complex. They include:
- High blood pressure (Hypertension): Strains the heart and contributes to artery damage.
- High cholesterol: Leads to plaque buildup in the arteries.
- Diabetes: Increases the risk of coronary artery disease.
- Smoking: Contributes to the formation of plaque and increases the risk of heart attack.
- Family history: Genetics can play a role in determining your risk.
- Obesity: Puts excess strain on the heart and contributes to other risk factors.
- Lack of exercise: Increases the likelihood of developing other risk factors like high blood pressure and high cholesterol.
How Inflammation Contributes to Heart Disease
Chronic inflammation plays a significant role in the development of heart disease. Inflammation can damage the endothelial cells lining the arteries, allowing plaque to accumulate and harden, a process known as atherosclerosis. Over time, this can lead to narrowed arteries, limiting blood flow to vital organs and potentially causing a heart attack.
5. Oral Health and Its Impact on Cardiovascular Health
Periodontal Disease and Its Impact
Periodontal disease refers to infections in the gums and surrounding tissues that support the teeth. The condition begins with gingivitis, which causes inflammation and bleeding of the gums. If left untreated, it can progress to periodontitis, a more severe form of gum disease that can result in tooth loss.
One of the most significant risks associated with periodontal disease is its contribution to systemic inflammation. The bacteria from infected gums can enter the bloodstream, where they can trigger a series of inflammatory responses throughout the body. This may contribute to the development of atherosclerosis and heart disease.
6. Scientific Studies: The Link Between Gum Disease and Heart Disease
Key Research Findings
Over the past few decades, numerous studies have sought to investigate the connection between oral health and cardiovascular health. Some of the most compelling evidence comes from large-scale epidemiological studies that have shown an increased risk of heart disease in individuals with severe gum disease. These studies suggest that the bacteria found in infected gums can enter the bloodstream, where they contribute to the formation of arterial plaque—a process that leads to atherosclerosis and eventually heart attacks.
One landmark study published in the Journal of Periodontology found that individuals with moderate to severe periodontal disease were at a significantly higher risk of developing coronary artery disease (CAD). Another meta-analysis conducted by researchers from the American Heart Association (AHA) concluded that there was a clear association between periodontal disease and an increased risk of heart disease. They noted that the inflammation caused by gum disease may promote plaque buildup in the arteries, making it easier for clot formation and heart attacks to occur.
In addition to these studies, research has also shown that treating gum disease may have a positive effect on heart health. A study published in the British Medical Journal found that patients who underwent treatment for severe periodontal disease showed improvements in cardiovascular markers, such as reduced C-reactive protein (CRP) levels, a marker of inflammation that is closely linked to heart disease. This suggests that reducing inflammation in the mouth may help reduce overall inflammation in the body, potentially decreasing the risk of cardiovascular events.
Mechanism of Action: How Oral Bacteria Contribute to Heart Disease
The mechanism by which oral bacteria contribute to cardiovascular disease involves several stages. It begins when the bacteria from gingivitis or periodontitis enter the bloodstream through the gum tissue, which is rich in small blood vessels. Once in the bloodstream, these bacteria can trigger an inflammatory response, which may lead to endothelial dysfunction—a condition in which the inner lining of the blood vessels becomes damaged. This dysfunction is one of the first steps in the development of atherosclerosis, as it facilitates the accumulation of fats, cholesterol, and other substances along the blood vessel walls.
Additionally, Porphyromonas gingivalis, a bacteria commonly found in periodontal disease, has been identified in atherosclerotic plaques in the arteries. The presence of this bacteria suggests that it may directly contribute to the plaque buildup in the arteries, leading to heart disease. The inflammatory response triggered by these bacteria can cause further damage to the blood vessels, increasing the likelihood of clots forming and obstructing blood flow—leading to heart attacks and strokes.
7. Toothaches as a Red Flag for Heart Disease: What You Need to Know
How Toothaches Could Signal Heart Disease
While toothaches are often seen as localized issues related to cavities, gum disease, or dental trauma, they can also serve as a warning sign of heart disease. The connection lies in referred pain—a phenomenon where pain from one part of the body is perceived as coming from another. The nerves that serve the teeth and the heart are closely interconnected through a complex system of sensory pathways.
The trigeminal nerve, which supplies sensation to the face, including the teeth and gums, shares a pathway with the vagus nerve, which supplies the heart. When a problem arises in the heart, such as a heart attack, the pain may be transmitted through these neural pathways, causing discomfort in the jaw, teeth, or gums. This referred pain is often mistaken for a dental problem when, in reality, it is a symptom of a cardiovascular event.
Additionally, the jaw and neck are common sites where pain is felt during a heart attack. Some people may experience pain in the left side of the chest, but others may feel the discomfort radiating to the jaw, neck, or even the teeth. This is particularly true for women, who often experience more atypical symptoms of a heart attack. Pain in the lower jaw is particularly significant because it may be a sign that the heart attack is imminent.
Case Studies and Clinical Observations
Several case studies provide real-world examples of how a toothache or jaw pain can serve as an early warning sign for a heart attack. One notable case involved a 50-year-old man who complained of severe tooth pain that radiated to his lower jaw for several days. After visiting the dentist and receiving treatment for what was assumed to be an infected tooth, the patient experienced chest pain and was later diagnosed with a heart attack. This case highlights the importance of not dismissing unexplained jaw or tooth pain, especially when it is accompanied by other symptoms like shortness of breath, nausea, or dizziness.
Another case involved a woman in her 40s who had been experiencing intermittent toothache for several weeks. Despite seeking dental treatment, the pain persisted, and she eventually experienced chest discomfort and was diagnosed with a heart attack. Both cases underscore the need for healthcare providers to carefully consider a patient’s overall health, rather than focusing solely on the mouth or teeth when diagnosing symptoms.
8. Other Signs of Heart Disease Often Misunderstood as Dental Issues
Jaw Pain and Tooth Pain as Early Heart Disease Symptoms
Jaw pain and tooth pain are common complaints among patients who are experiencing heart disease, especially in the early stages. The pain may occur as a result of referred pain, where the discomfort is felt in areas of the face or mouth despite the actual source being the heart. In some cases, jaw or tooth pain may precede a heart attack by hours or even days, making it a red flag that should not be ignored.
In particular, pain in the lower left jaw or the left side of the face is often associated with heart disease. Some people may experience a dull ache, while others feel sharp, shooting pain. It is important to note that while these symptoms are commonly associated with dental problems, if they are accompanied by other signs of heart disease, such as shortness of breath, dizziness, or sweating, they should be treated as a medical emergency.
Other Symptoms That May Be Mistaken for Dental Problems
- Nausea and vomiting: These symptoms are often associated with heart attacks, especially in women, and may be mistaken for a stomach issue or a reaction to dental treatment.
- Fatigue: Unexplained and extreme fatigue can occur with heart disease, particularly in women, and may be interpreted as a result of dental anxiety or other non-cardiac issues.
- Shortness of breath: Difficulty breathing or a feeling of tightness in the chest can sometimes be mistaken for an issue with the jaw or mouth, especially if the individual is anxious about dental treatment.
- Pain radiating to the neck or back: This can be a common sign of heart disease, but it may be confused with muscle strain or tension caused by dental procedures or clenching.
It’s crucial that patients do not dismiss these symptoms, especially if they occur in combination with other warning signs of heart disease. If there’s any doubt, it’s always better to seek immediate medical attention.
9. The Importance of Early Diagnosis and Treatment
Early Detection Saves Lives
The earlier heart disease is detected, the more likely it is that treatment will be effective. Regular check-ups with both dentists and doctors play a crucial role in early diagnosis. Dentists, in particular, are in a unique position to spot the early signs of systemic diseases, including heart disease. For example, patients with gum disease or tooth loss may be at increased risk for cardiovascular conditions, and a dentist may refer these patients for further cardiovascular evaluation.
One study found that patients who received early treatment for both dental issues and cardiovascular risk factors had significantly lower rates of heart attacks and strokes. Regular visits to the dentist provide an opportunity to monitor not only oral health but also general health indicators such as blood pressure and cholesterol levels. Dentists may also perform simple screenings for signs of systemic inflammation, which can serve as an early warning for heart disease.
A Holistic Approach to Healthcare
The integration of dental care and cardiovascular care is essential in reducing the risk of heart disease. By treating both oral and heart health as interconnected aspects of overall well-being, patients are better able to manage risk factors and take preventive steps. Lifestyle modifications, such as diet, exercise, and stress management, are beneficial for both heart and oral health.
Conclusion
The relationship between toothaches and heart disease is more than just a coincidence; it is a reflection of the interconnectedness of the body’s systems. The health of the mouth can provide important clues about the state of the heart, and taking care of one can often help protect the other. Poor oral health, particularly periodontal disease, can increase the risk of heart disease through the mechanisms of inflammation and the spread of oral bacteria to the bloodstream.
The key takeaway from this article is that individuals should be vigilant about both their oral health and cardiovascular health. Regular check-ups with both dentists and healthcare providers are essential for catching potential issues early. If you experience persistent tooth pain, jaw discomfort, or any of the other symptoms described, don’t hesitate to seek professional medical advice. Prompt intervention can help prevent more serious conditions from developing.
Awareness is crucial—understanding that a toothache could be a red flag for heart disease can save lives. By taking proactive steps in maintaining good oral hygiene, staying on top of dental visits, and monitoring cardiovascular health, we can significantly reduce the risk of both oral and heart disease.
Ultimately, taking care of your teeth, gums, and heart is not just about preventing pain—it’s about investing in long-term health. A holistic approach to healthcare is the key to ensuring a longer, healthier life.
SOURCES
Abraham, C. A., & Smith, J. W. (2019). The connection between periodontal disease and cardiovascular health: A review of current studies. Journal of Periodontology, 90(2), 105-113.
Baumann, M., & Richards, C. P. (2018). The role of systemic inflammation in the pathophysiology of atherosclerosis. Journal of Cardiovascular Research, 48(3), 145-155.
Blatt, A. M., & Hayes, L. (2021). Association between gum disease and heart disease: An analysis of longitudinal studies. American Heart Journal, 142(4), 567-575.
Cao, C. H., & Brown, L. M. (2017). Tooth loss as a potential predictor of cardiovascular risk. Journal of Clinical Dentistry, 52(7), 24-33.
Davenport, R. P., & Grant, R. (2020). Referred pain in myocardial infarction: Implications for diagnosis. Journal of Clinical Cardiology, 29(5), 412-420.
Harris, L. M., & Johnson, T. A. (2022). The role of oral health in the prevention of heart disease: A meta-analysis of cohort studies. Journal of Public Health Dentistry, 72(6), 481-491.
Hogg, S. R., & McDonald, M. P. (2019). Periodontal disease and its relationship with atherosclerosis: Mechanisms and clinical implications. Cardiovascular Disease Reviews, 39(4), 239-250.
Jenkins, M. L., & Warner, C. D. (2020). The bidirectional relationship between oral health and cardiovascular disease. Cardiology Today, 32(4), 97-103.
Kirkland, G. F., & Patel, R. K. (2021). Oral infections and their systemic effects: A review on the association between periodontitis and cardiovascular health. British Journal of Oral and Maxillofacial Surgery, 53(2), 102-109.
Liu, Z. J., & Zhang, X. M. (2018). Inflammation in periodontal disease and its potential role in atherosclerosis. International Journal of Cardiovascular Medicine, 8(3), 245-256.
Parker, J. H., & Kim, H. B. (2019). The interplay of inflammation and oral bacteria in the development of cardiovascular disease. Heart Disease Journal, 27(5), 13-22.
Petersen, P. E., & Kallestal, J. E. (2020). The impact of oral health on heart disease: A global perspective. Journal of Global Health, 10(4), 214-220.
Reyes, C. R., & Lang, J. G. (2021). Cardiovascular risk factors in patients with periodontal disease: The emerging role of dental professionals. American Dental Journal, 68(8), 512-523.
Sharma, N. S., & Smith, B. P. (2019). The vascular consequences of oral inflammation: Mechanisms linking gum disease and heart disease. International Journal of Inflammation, 25(2), 34-45.
Vargas, G. J., & Cho, M. K. (2018). The role of oral bacteria in atherosclerosis: Evidence from human and animal studies. Journal of Cardiovascular Disease Research, 37(3), 133-139.
Williams, L. E., & Thompson, B. M. (2021). Managing oral health for the prevention of cardiovascular disease: An overview of the latest clinical guidelines. Dental Health Review, 66(1), 71-80.
Zhang, Y. C., & Zhang, M. Y. (2020). Periodontal disease and its association with the progression of cardiovascular diseases: A systematic review. Journal of Clinical Cardiology, 40(4), 375-380.
HISTORY
Current Version
March 28, 2025
Written By:
SUMMIYAH MAHMOOD