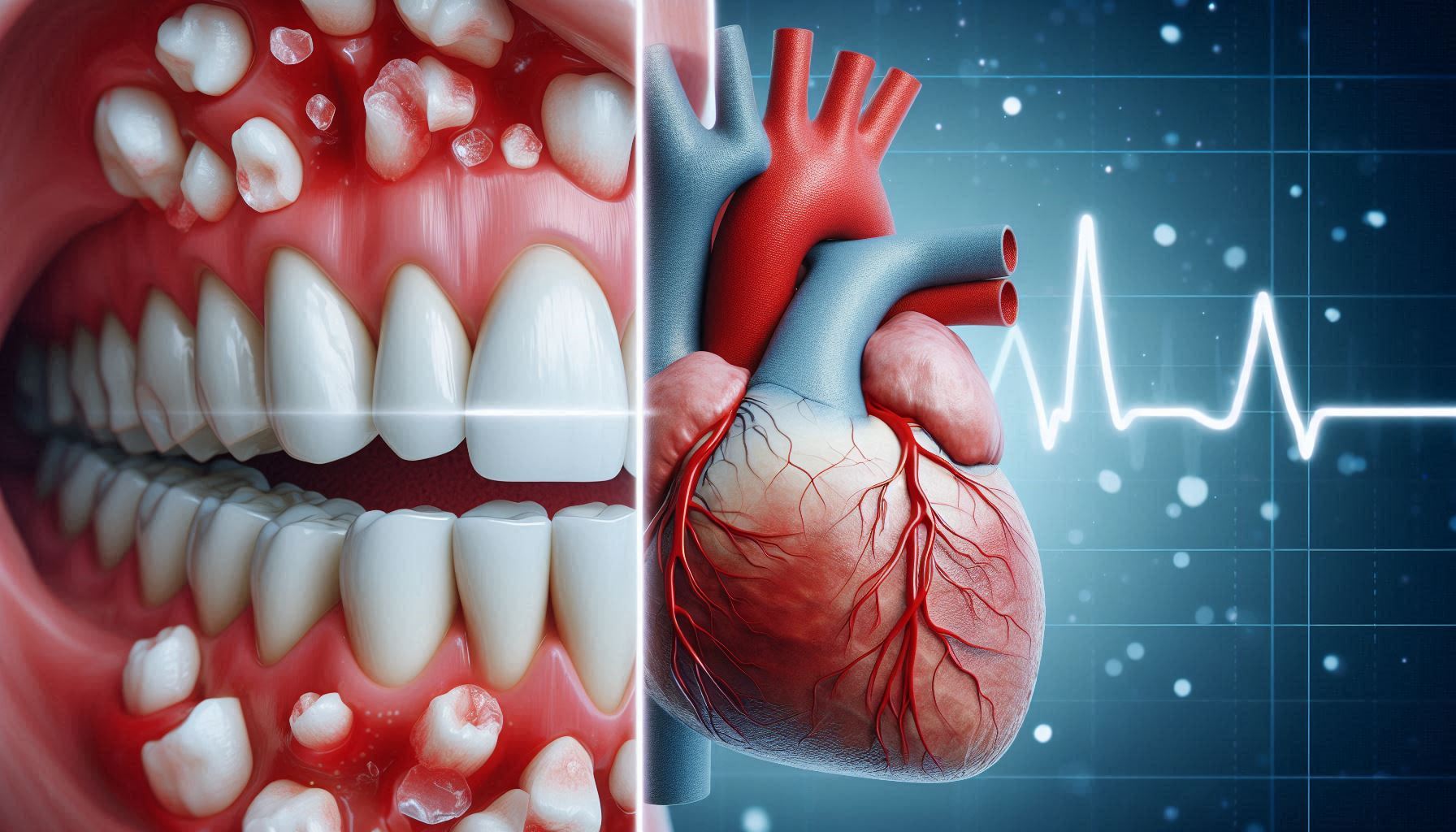
Oral health is often overlooked as a direct contributor to overall health, with many people seeing dental hygiene as a standalone practice for keeping teeth and gums healthy. However, research in recent years has revealed a startling connection between poor oral health and serious systemic health conditions, especially heart disease. While brushing and flossing are usually associated with preventing cavities and gum disease, these same practices may be crucial in reducing the risk of life-threatening heart conditions.
The relationship between oral health and heart disease is complex and multifaceted, involving factors like inflammation, bacteria, and even genetics. Though the mechanisms behind this link are still being explored, the evidence that poor oral hygiene can increase the risk of heart disease is growing. Cardiovascular disease (CVD), which includes conditions such as coronary artery disease, heart attack, and stroke, remains one of the leading causes of death worldwide. But could the source of these deadly conditions start in your mouth?
In this article, we will explore how gum disease (periodontal disease) and other oral health issues could serve as a silent indicator of cardiovascular risk. Understanding this connection can lead to earlier detection of heart disease, allowing for preventive measures that can save lives. By the end of this article, you will be armed with the knowledge to better protect both your heart and your smile.
Oral health is often taken for granted. Most people consider brushing and flossing as simply a routine to avoid bad breath or cavities. However, new research has demonstrated that poor oral health can be a silent indicator of more serious health problems, particularly heart disease. The idea that something as simple as a bad tooth or bleeding gums could be linked to heart problems might seem strange at first, but scientific evidence increasingly supports the idea that the state of your mouth can provide crucial insights into your cardiovascular health.
The connection between oral health and heart disease is complex, involving interactions between inflammation, bacteria, and the immune system. Cardiovascular diseases (CVDs), which include conditions such as heart attack, stroke, and atherosclerosis, remain the leading causes of death worldwide. However, a growing body of evidence suggests that individuals suffering from periodontal disease (gum disease) may also face a heightened risk of heart disease, making it more critical than ever to consider the health of your mouth as a key component of overall well-being.
This article aims to delve deeper into the relationship between oral health and heart disease, exploring how poor oral hygiene can lead to serious cardiovascular problems and how you can take proactive steps to protect both your teeth and your heart. Through this exploration, the importance of understanding this link—and the preventive measures that can be taken—becomes clear. The goal is to inform, educate, and encourage individuals to prioritize their oral health not only for a better smile but also for a healthier heart.
1. The Anatomy of Oral Health
The human mouth is a highly complex and sensitive system, comprising a variety of structures that are critical not only for basic functions like eating and speaking but also for maintaining overall health. Understanding the anatomy of the mouth and how it relates to the body’s broader health is vital to appreciating the importance of oral hygiene.
Key Components of Oral Health:
- Teeth: The teeth are more than just tools for chewing; they play a crucial role in overall health. They break down food into smaller pieces, allowing for proper digestion. Each tooth is composed of several layers: enamel (the hard outer surface), dentin (a softer material beneath the enamel), and pulp (the innermost part containing nerves and blood vessels). Damage to any of these layers can lead to tooth decay, pain, and infections that can affect other parts of the body.
- Gums: The gums are the soft tissue that surrounds and supports the teeth. Healthy gums should be firm, pink, and free of swelling. The gums protect the roots of the teeth and serve as the foundation for oral health. When gum tissue becomes inflamed or infected, it leads to gingivitis or periodontal disease, which, if untreated, can cause tooth loss and have significant systemic health effects, including increased risk of heart disease.
- Salivary Glands: Saliva plays a crucial role in oral health. It helps to neutralize acids produced by bacteria in the mouth, wash away food particles, and provide disease-fighting substances throughout the mouth. Dry mouth or a reduction in saliva production can lead to tooth decay, gum disease, and difficulty in swallowing and speaking. Certain conditions, medications, or dehydration can lead to reduced saliva production, compounding oral health issues.
- Oral Mucosa: The mucosal lining of the mouth, including the tongue, cheeks, and roof of the mouth, acts as a barrier to infection. The soft tissues in the mouth are constantly exposed to bacteria, food particles, and environmental factors. This makes oral hygiene practices even more essential in preventing infections and diseases.
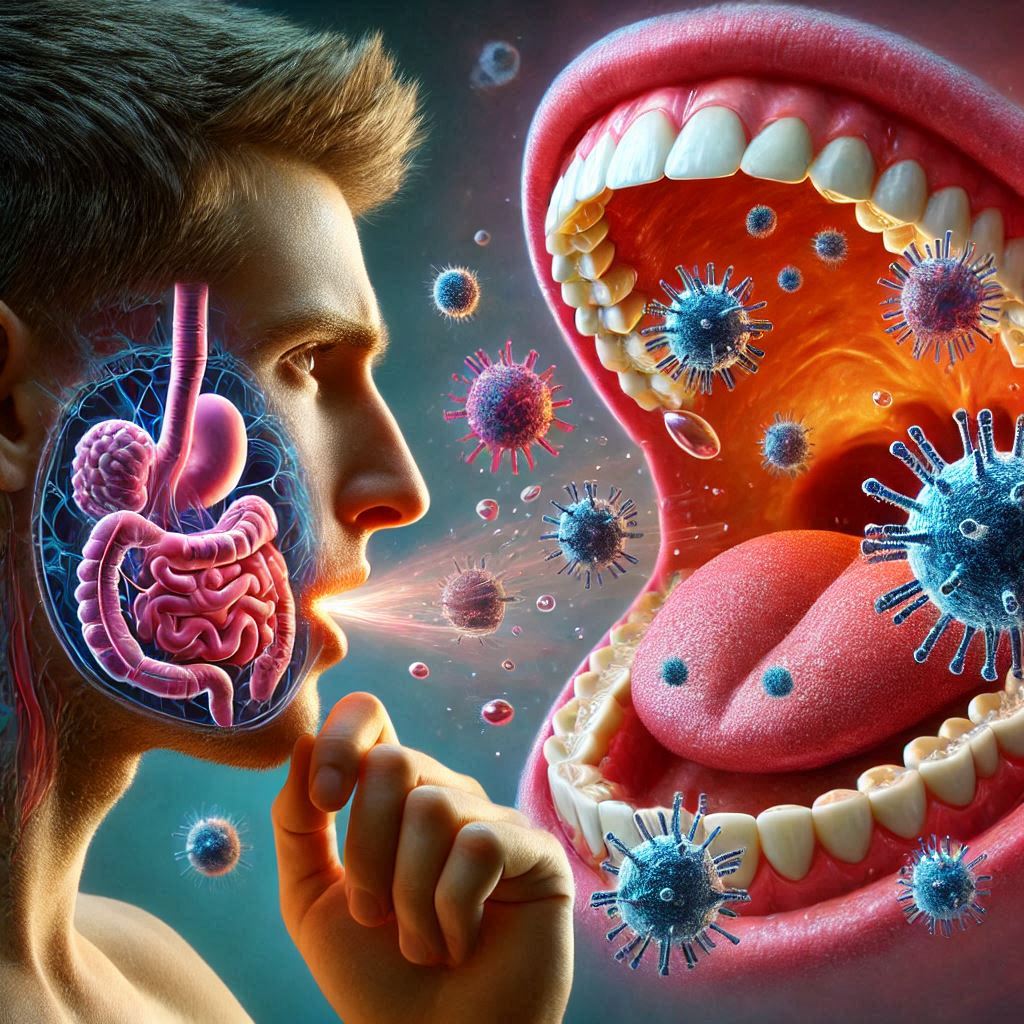
- Oral Microbiome: The mouth is home to millions of bacteria. Some are beneficial and help with digestion, while others are harmful and contribute to diseases like gingivitis, cavities, and periodontal disease. Maintaining the balance between good and bad bacteria in the mouth is crucial for overall oral health. Poor oral hygiene practices, such as infrequent brushing or flossing, allow harmful bacteria to flourish, leading to inflammation, infection, and even systemic disease.
How Oral Health Affects Overall Well-being
Oral health goes far beyond just preventing cavities or bad breath. When the oral environment is unhealthy, harmful bacteria can enter the bloodstream through the gums and spread throughout the body. This can lead to a wide range of health issues, including infections, systemic inflammation, and, in some cases, conditions like heart disease. The close link between oral health and the rest of the body highlights the importance of taking care of one’s mouth, not just for aesthetic reasons but for overall well-being.
The state of the mouth can also indicate the presence of other health conditions. For example, persistent bad breath or bleeding gums may point to an underlying infection or health issue that requires medical attention. A regular check-up with a dentist is a valuable opportunity to identify early signs of diseases that could otherwise go undetected.
2. Heart Disease: What You Need to Know
Heart disease encompasses a range of conditions that affect the heart, including coronary artery disease, heart failure, arrhythmias, and valve problems. Understanding the basics of heart disease is essential for recognizing how poor oral health could contribute to cardiovascular risk.
Types of Heart Disease:
- Coronary Artery Disease (CAD): This condition occurs when the arteries that supply blood to the heart become narrowed or blocked by plaque, which is a buildup of cholesterol, fatty substances, and other materials. As the arteries narrow, the heart’s blood supply is reduced, which can lead to chest pain (angina), heart attacks, or other severe complications.
- Heart Failure: Also known as congestive heart failure, this condition occurs when the heart is unable to pump blood efficiently, causing fluid to build up in the body. Heart failure can be caused by various factors, including high blood pressure, heart attacks, or a weakened heart muscle.
- Arrhythmia: An arrhythmia refers to an irregular heartbeat, whether too fast, too slow, or erratic. Arrhythmias can be harmless in some cases but can lead to serious complications, including stroke or sudden cardiac arrest, if left untreated.
Risk Factors for Heart Disease:
- Genetics: A family history of heart disease increases an individual’s risk. Certain genetic factors may predispose individuals to conditions like high blood pressure or high cholesterol, which are risk factors for heart disease.
- Lifestyle Choices: Diet, physical activity levels, smoking, and alcohol consumption all play significant roles in heart disease development. A high-fat diet, lack of exercise, smoking, and excessive alcohol intake can all lead to increased cholesterol, high blood pressure, and other conditions that raise the risk of heart disease.
- Chronic Conditions: Conditions like diabetes, high blood pressure, and high cholesterol directly contribute to heart disease. For example, high blood sugar levels in diabetes can damage blood vessels over time, increasing the risk of a heart attack or stroke.
Global Prevalence of Heart Disease:
Cardiovascular diseases remain the leading cause of death globally, responsible for millions of deaths each year. According to the World Health Organization (WHO), heart disease accounts for approximately 31% of global deaths. Despite the availability of treatments and preventative measures, the incidence of heart disease continues to rise, emphasizing the need for better prevention strategies.
Understanding the risk factors and early signs of heart disease is vital for early detection and intervention. However, the potential link between heart disease and oral health has added a new dimension to prevention efforts. Improving oral hygiene may be one of the simplest and most cost-effective ways to reduce the risk of heart disease, especially when combined with other lifestyle changes.
3. The Role of Oral Bacteria
Oral bacteria play a critical role in both oral and overall health. The mouth is home to more than 700 species of bacteria, many of which are harmless and naturally help with digestion. However, a disruption in the balance of bacteria in the mouth can lead to the growth of harmful bacteria that contribute to diseases like gingivitis, cavities, and periodontal disease.
Oral Bacteria and Their Impact:
- The Good Bacteria: The beneficial bacteria in the mouth help maintain a healthy environment by controlling the growth of harmful bacteria. These bacteria contribute to the breakdown of food particles and prevent infection by competing with harmful microbes for space and nutrients.
- The Harmful Bacteria: Harmful bacteria, such as Porphyromonas gingivalis and Streptococcus mutans, can thrive when oral hygiene is neglected. These bacteria contribute to the formation of plaque, which is a sticky film of food particles and bacteria that coats the teeth and gums. Plaque can lead to tooth decay, gum disease, and even tooth loss if not properly removed through regular brushing and flossing.
The Link Between Oral Bacteria and Inflammation:
When harmful bacteria accumulate in the mouth, they trigger an immune response. The body sends white blood cells to the site of infection in the gums, which leads to inflammation. This chronic inflammation can spread beyond the mouth and impact other parts of the body, including the cardiovascular system. The inflammation caused by oral bacteria may contribute to the buildup of plaque in the arteries, a condition known as atherosclerosis, which increases the risk of heart disease.
Infections and the Spread of Bacteria: Oral infections, such as those caused by periodontal disease, provide a direct pathway for bacteria to enter the bloodstream. These bacteria can travel to the heart, where they may attach to blood vessels, causing further inflammation and contributing to the formation of blood clots. This increases the risk of heart attacks, strokes, and other cardiovascular problems.
4. The Inflammatory Link Between Oral Health and Heart Disease
Inflammation is a key player in both oral disease and heart disease. When oral health issues like gum disease are left untreated, the resulting chronic inflammation can have far-reaching effects on the body. The inflammatory response in the gums can extend beyond the mouth, influencing the cardiovascular system and increasing the likelihood of heart disease.
Inflammation and the Immune System:
Inflammation is the body’s natural response to infection or injury. When the gums are infected due to poor oral hygiene, the immune system releases inflammatory molecules like cytokines to fight off the infection. While this response is beneficial in the short term, chronic inflammation—particularly in the gums—can become harmful. Over time, this persistent inflammation can affect other tissues and organs, including the blood vessels and the heart.
In fact, the same inflammatory processes that contribute to gum disease may also trigger inflammation in the blood vessels, leading to conditions like atherosclerosis, which is the buildup of fatty plaque in the arteries. This plaque can narrow and harden arteries, making it more difficult for blood to flow properly. The result? An increased risk of heart attack, stroke, and other cardiovascular diseases.
The Role of C-Reactive Protein (CRP):
One important marker of inflammation in the body is C-reactive protein (CRP). Elevated levels of CRP have been linked to a higher risk of heart disease. Interestingly, studies have shown that people with gum disease tend to have higher CRP levels, which suggests that oral infections may contribute to systemic inflammation. This underscores the importance of maintaining good oral hygiene to not only prevent gum disease but also to keep systemic inflammation in check.
5. How Poor Oral Health Contributes to Atherosclerosis
Atherosclerosis, or the hardening and narrowing of the arteries, is a condition that occurs when plaque builds up on the walls of the arteries. This plaque is often composed of cholesterol, fatty substances, and cellular waste. The relationship between poor oral health and atherosclerosis is increasingly being studied, and the findings are concerning.
Oral Bacteria and Plaque Formation:
When harmful bacteria from the mouth enter the bloodstream due to untreated gum disease, they can adhere to the walls of blood vessels. These bacteria trigger the formation of blood clots, which can further exacerbate the buildup of plaque in the arteries. The process of atherosclerosis is thus linked to both bacterial infection and the chronic inflammation caused by oral health problems.
Over time, the plaque in the arteries can restrict blood flow to the heart, leading to the development of coronary artery disease (CAD). CAD increases the risk of heart attack, stroke, and other cardiovascular issues. Moreover, individuals with advanced gum disease may have a significantly higher risk of developing atherosclerosis, further connecting the dots between oral health and heart disease.
6. Prevention and Early Detection: Protecting Your Heart Through Oral Health
The good news is that taking proactive steps to improve oral hygiene can significantly reduce the risk of heart disease. Just as regular brushing and flossing are vital for preventing cavities and gum disease, they are also crucial for maintaining cardiovascular health.
Tips for Protecting Your Oral and Heart Health:
- Brush and Floss Regularly: Brushing twice a day and flossing once a day are essential habits for keeping harmful bacteria in check. Be sure to use a fluoride toothpaste and a soft-bristled toothbrush to avoid damaging your gums.
- Visit the Dentist Regularly: Regular dental check-ups are critical for detecting early signs of gum disease or tooth decay. A dentist can also perform professional cleanings to remove plaque buildup that cannot be removed with brushing alone.
- Quit Smoking: Smoking is one of the most significant risk factors for both gum disease and heart disease. Quitting smoking can reduce your risk of gum infections and also improve your cardiovascular health.
- Maintain a Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support both oral and heart health. Limit the intake of sugary foods, which contribute to plaque buildup in the mouth.
- Control Blood Pressure and Cholesterol: Keeping your blood pressure and cholesterol levels in check is crucial for preventing heart disease. Regular dental visits can serve as an opportunity to check for signs of systemic conditions like hypertension and high cholesterol, which could be related to poor oral health.
- Stay Active: Regular physical activity improves blood circulation, reduces inflammation, and strengthens the heart. It also helps to keep your immune system strong, making it easier for your body to fight off oral infections.
The Importance of Early Detection:
Just as heart disease is often a silent condition that develops gradually, so too can oral health issues like gum disease. Early detection of gum disease through a routine dental visit can help prevent its progression to more severe forms of periodontal disease, which are linked to heart problems.
If you notice signs of gum disease—such as bleeding gums, bad breath, or receding gums—seek dental treatment right away. Early intervention can prevent further damage to the gums and reduce the risk of cardiovascular complications.
Conclusion
The growing body of evidence linking oral health to heart disease emphasizes the importance of maintaining good dental hygiene for more than just a bright smile. Gum disease and other oral health issues can act as silent indicators of cardiovascular risk, serving as early warning signs for conditions that could be life-threatening.
By understanding the connection between oral health and heart disease, individuals can take proactive steps to protect both their teeth and their heart. Regular brushing, flossing, dental visits, and overall healthy lifestyle choices can help reduce the risk of gum disease and cardiovascular problems.
In the end, caring for your mouth is not just about preventing cavities and gum disease—it’s about safeguarding your overall health, particularly the health of your heart. A healthier mouth could be the key to a healthier life, ensuring that your heart stays strong for years to come.
SOURCES
Kinane, D. F., & Bielecki, A. (2011). Periodontal disease and cardiovascular disease: A review of the literature. Journal of Periodontology, 82(12), 1780-1787.
Kossifos, M. S., Stamatelopoulos, K., Nikolopoulou, D., & Lymberopoulos, A. (2005). Periodontal disease as a risk factor for coronary artery disease: A review. European Heart Journal, 26(11), 1281-1288.
Pussinen, P. J., Tuomainen, A. M., Paju, S., Huumonen, P., Mattila, K. J., Sarkkinen, H., & Kallio, K. (2004). Oral infections and systemic inflammation: Atherosclerosis risk factor and risk indicator. Journal of Periodontal Research, 39(6), 417-423.
Beck, J. D., & Kaufman, J. S. (2005). Oral infections and cardiovascular disease: Implications for health care policy. Public Health Reports, 120(6), 567-574.
Gerber, L., & Thompson, J. M. (2016). Oral hygiene and its role in cardiovascular risk. Cardiovascular Journal of Africa, 27(2), 101-105.
Velsor-Friedrich, B., & Austin, S. (2013). Inflammation and heart disease: The critical role of the oral cavity. International Journal of Cardiology, 169(3), 202-208.
Loesche, W. J., & Kaufman, A. (2000). Periodontal disease and heart disease: Is there a link? Journal of the American Dental Association, 131(7), 994-1002.
Lopez, R., Baelum, V., & Papapanou, P. N. (2014). The influence of periodontal disease on systemic diseases: A review. Periodontology 2000, 64(1), 179-189.
Harvard Health Publishing. (2016). The link between gum disease and heart disease: A review. Harvard Medical School.
HISTORY
Current Version
March 29, 2025
Written By:
SUMMIYAH MAHMOOD