Understanding Gum Infections
1. What Are Gum Infections?
Gum infections, also known as periodontal disease, are bacterial infections that affect the tissues surrounding and supporting your teeth. These infections occur when plaque, a sticky, colorless film of bacteria, accumulates on the teeth and gums. If plaque isn’t removed by brushing and flossing, it hardens into tartar, which can only be removed by a dentist or dental hygienist. The presence of tartar can irritate the gums, causing them to become inflamed.
Types of Gum Infections:
- Gingivitis: This is the earliest stage of gum disease and is typically characterized by red, swollen gums that may bleed when brushing or flossing. Gingivitis is generally mild and can often be reversed with good oral hygiene practices like regular brushing and flossing.
- Periodontitis: If gingivitis isn’t treated, it can progress into periodontitis, a more severe form of gum disease. Periodontitis involves deeper infection of the gums, leading to gum recession and the formation of pockets between the teeth and gums where bacteria thrive. If left untreated, periodontitis can cause tooth loss and even damage to the bones supporting the teeth.
- Advanced Periodontitis: In the final stage, the infection may cause significant damage to the bone and tissue, resulting in tooth mobility or loss. At this stage, dental treatments may include surgery, bone grafts, or other invasive procedures to restore gum health.
Symptoms of Gum Infections:
- Bleeding gums, especially when brushing or flossing.
- Swollen, red, or tender gums.
- Persistent bad breath (halitosis).
- Receding gums or teeth that appear longer than usual.
- Loose teeth or tooth loss in advanced cases.
- Pus around the teeth or gums.
- A change in the fit of dentures or bridges.
2. How Do Gum Infections Develop?
Gum infections develop as a result of a combination of poor oral hygiene, the presence of bacteria, and the body’s inflammatory response. Here’s how it works:
- Plaque Buildup: The mouth naturally harbors bacteria, and when food particles and saliva combine, they form plaque on your teeth. If plaque is not removed regularly, it hardens into tartar, which irritates the gums.
- Gum Inflammation: The body’s immune system detects the presence of bacteria and begins an inflammatory response. This leads to swelling, redness, and bleeding of the gums—symptoms of gingivitis. Without proper care, the inflammation can worsen and lead to more severe infection.
- Progression to Periodontitis: As the infection spreads, it moves deeper into the gum tissues and affects the ligaments and bone that support the teeth. This can lead to periodontal pockets, which trap even more bacteria, exacerbating the infection and causing bone loss over time.
Risk Factors for Gum Infections: Several factors can increase the risk of developing gum infections, including:
- Poor oral hygiene: Inconsistent brushing or flossing allows plaque to build up on teeth and gums.
- Smoking: Tobacco use weakens the immune system, making it harder for the body to fight infections.
- Diabetes: High blood sugar levels can reduce the body’s ability to fight infection and promote inflammation in the gums.
- Age: The older you get, the more likely you are to develop gum disease, especially if you haven’t maintained good oral care.
- Genetics: Some people may be more genetically predisposed to gum disease due to inherited traits.
- Medications: Certain medications, such as those that cause dry mouth, can increase the risk of gum infections by reducing saliva, which helps protect the gums.
3. Stages of Gum Infections
Understanding the stages of gum disease is crucial for early detection and effective treatment. Here’s a breakdown of the progression:
- Gingivitis (Early Stage):
- Gingivitis is the mildest form of gum disease and is reversible with proper care.
- Gums become inflamed, and you may notice bleeding while brushing or flossing. There is typically no pain at this stage.
- Plaque accumulation is the primary cause.
- Early Periodontitis (Moderate Stage):
- As gingivitis progresses, it becomes periodontitis. This stage involves deeper infection, and the gums may begin to pull away from the teeth.
- Bacteria in the pockets between the teeth and gums begin to attack the bone and connective tissue that support the teeth.
- Treatment at this stage may require professional cleaning by a dentist or hygienist to remove tartar and bacteria from beneath the gumline.
- Advanced Periodontitis (Severe Stage):
- At this stage, the infection has caused significant damage to the bone and connective tissue that hold the teeth in place.
- Gums may recede significantly, leading to loose teeth and, in some cases, tooth loss.
- Surgical treatments may be required to restore gum health and prevent further damage.
The Role of Inflammation in Gum Disease
1. What is Inflammation?
Inflammation is the body’s natural response to injury, infection, or harmful stimuli. It’s a protective mechanism that helps the body fight off infections and repair tissue damage. In the case of gum infections, the body’s immune system recognizes bacteria in the gums and triggers an inflammatory response to neutralize the threat.
However, while acute inflammation is essential for healing, chronic inflammation—which occurs when the body continues to fight an infection without resolution—can have damaging effects. In the case of periodontal disease, chronic inflammation can harm the tissues and structures that support the teeth, leading to gum recession, tooth mobility, and even loss of teeth.
2. Chronic Inflammation and Heart Disease
The connection between chronic inflammation in the gums and heart disease is an emerging area of research. Here’s how it works:
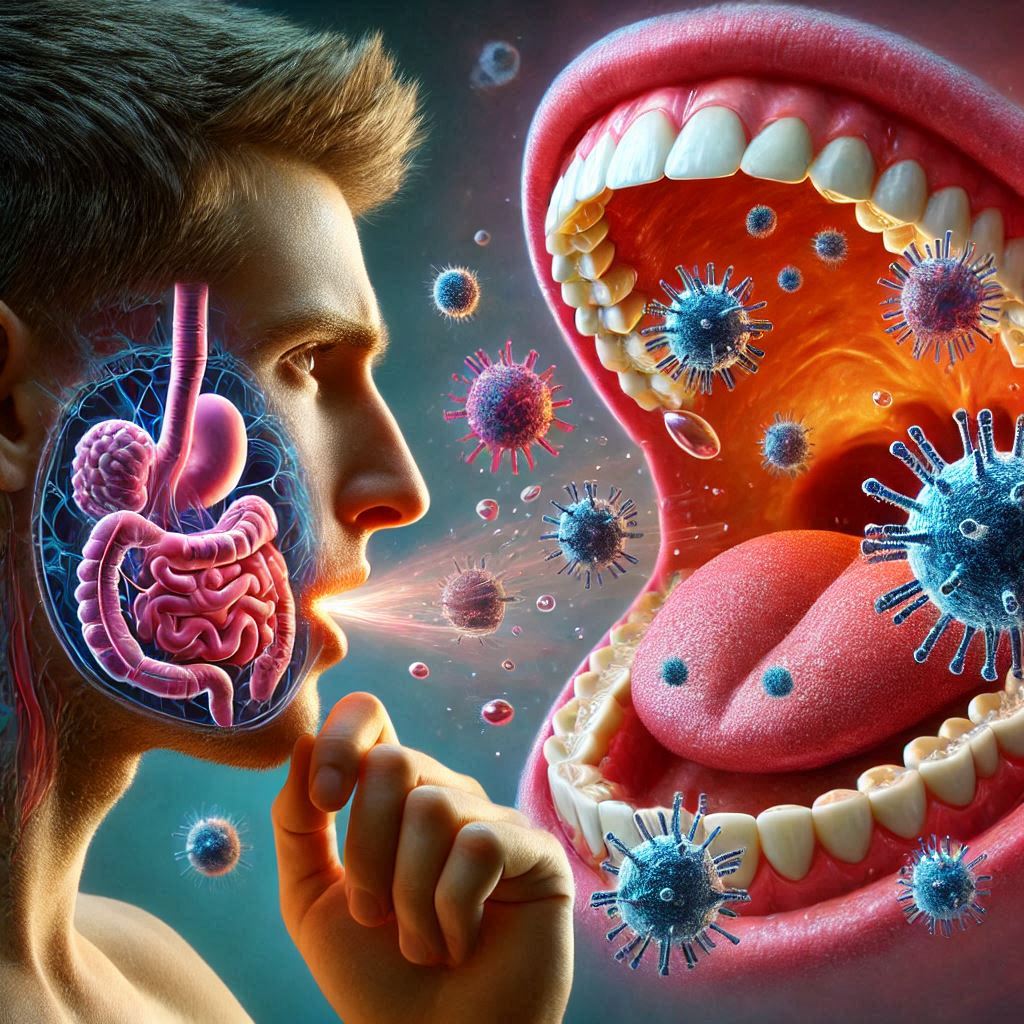
- Systemic Inflammation: The bacteria causing gum infections don’t stay confined to the mouth. They can enter the bloodstream through tiny blood vessels in the gums, especially when the gums are inflamed and damaged. Once in the bloodstream, these bacteria can travel to other parts of the body, including the heart.
- Atherosclerosis: When the bacteria from infected gums enter the bloodstream, they can trigger an immune response that causes inflammation in blood vessels. This inflammation contributes to the formation of atherosclerotic plaques—fatty deposits that build up in the arteries, narrowing and hardening them. Over time, this process can lead to atherosclerosis, a condition where the arteries become blocked or narrowed, restricting blood flow.
- Risk of Heart Disease: Atherosclerosis is a major risk factor for heart disease, as it can lead to coronary artery disease (CAD), heart attacks, and strokes. Essentially, the chronic inflammation from gum disease contributes to the development of the very conditions that threaten heart health.
3. The Immune System Response
The body’s immune response to a gum infection is complex. When the immune system detects harmful bacteria, it sends white blood cells to fight the infection. This triggers the release of various molecules, including cytokines (inflammatory proteins) and prostaglandins (chemicals that mediate inflammation). While these molecules are essential for fighting infection, they can also harm tissues if their production becomes excessive.
In the context of periodontal disease, these inflammatory molecules can not only damage the gums and bone but also contribute to the systemic inflammation that affects the entire body, including the cardiovascular system. This systemic inflammation is what links gum infections to heart disease.
3. The Heart Disease Connection
1. How Can Gum Infections Affect Heart Health?
Now, let’s explore how the bacteria from infected gums can directly impact heart health.
- Bacterial Invasion: The mouth is home to millions of bacteria, and when the gums are infected, some of these bacteria can enter the bloodstream through small tears or openings in the gum tissue. This process is known as bacteremia.
- Heart Inflammation: Once in the bloodstream, these bacteria can travel to the heart and cause inflammation. In some cases, the bacteria can even infect the inner lining of the heart (the endocardium), potentially leading to a serious condition called infective endocarditis, though this is relatively rare.
- Atherosclerosis and Plaque Formation: Chronic low-level inflammation caused by gum disease can accelerate the process of plaque formation in the arteries. As the plaque builds up, it narrows the arteries, restricting blood flow. Over time, this process can lead to atherosclerosis and increase the risk of heart attacks, strokes, and other cardiovascular diseases.
- Blood Clotting: Some of the inflammatory molecules released by the immune system in response to gum infections can also increase the likelihood of blood clot formation. When blood clots form in narrowed arteries, they can block blood flow to the heart or brain, causing a heart attack or stroke.
2. Scientific Research and Evidence
A growing body of research has confirmed the connection between periodontal disease and heart disease. Here are some key studies:
- A study by the American Heart Association (AHA) found that people with gum disease are nearly twice as likely to suffer from coronary artery disease (CAD) as those without gum disease. The researchers hypothesized that the inflammation caused by gum disease contributes to the buildup of plaque in the arteries.
- Another study published in the Journal of the American College of Cardiology suggested that treating gum disease can help reduce overall inflammation in the body, potentially lowering the risk of heart disease.
- The Lancet Journal of Infectious Diseases published a meta-analysis that reviewed multiple studies and found a significant link between periodontal disease and an increased risk of heart attack, stroke, and other cardiovascular events. This research supports the idea that the inflammatory processes triggered by gum infections can have far-reaching effects on cardiovascular health.
3. Potential Mechanisms Behind the Connection
There are several theories about the exact mechanisms that link gum infections to heart disease:
- Direct Infection: In some cases, the bacteria from gum infections may directly infect the heart or other blood vessels. This could trigger further inflammation in the cardiovascular system, increasing the risk of heart disease.
- Systemic Inflammation: More commonly, the systemic inflammation triggered by gum disease leads to the development of atherosclerosis and other cardiovascular problems. The bacteria and inflammatory molecules from the gums can spread throughout the body, exacerbating existing risk factors for heart disease, such as high cholesterol, high blood pressure, and diabetes.
- Elevated C-Reactive Protein (CRP): Chronic inflammation from gum disease may also lead to elevated levels of C-reactive protein (CRP), a marker of inflammation in the body. High CRP levels are associated with an increased risk of heart disease, and studies have shown that people with periodontal disease tend to have higher CRP levels than those without.
4. How Your Dentist Can Detect and Help Prevent Heart Disease
1. Dentists as a First Line of Defense
Dentists are often the first healthcare providers to notice signs of gum disease. During a routine dental exam, your dentist can detect early warning signs of gum disease that could indicate a risk for heart disease. Regular checkups are essential, as dentists are trained to recognize subtle signs of inflammation or infection in the gums that might otherwise go unnoticed.
2. Early Warning Signs Your Dentist May Notice
- Bleeding Gums: One of the most common signs of gum disease. If your gums bleed while brushing or flossing, it may indicate gingivitis or more severe periodontal disease.
- Bad Breath (Halitosis): Persistent bad breath or a bad taste in the mouth is another sign of gum infection.
- Loose Teeth: As the disease progresses, the gums may recede and cause the teeth to become loose.
- Changes in Bite: A change in how your teeth fit together when you bite could indicate advanced gum disease and bone loss.
3. The Importance of Regular Checkups
By visiting your dentist regularly, you can detect gum disease in its earliest stages when it’s most treatable. In addition to cleaning your teeth and gums, your dentist may recommend regular periodontal screenings to monitor the health of your gums and identify any signs of inflammation or infection.
4. Collaborating with Other Healthcare Providers
Dentists can collaborate with cardiologists and other healthcare providers to offer a more comprehensive approach to patient care. If a dentist identifies symptoms of gum disease, they may refer you to a cardiologist for further testing, especially if you have risk factors for heart disease. This collaboration can help catch potential health issues early and improve overall health outcomes.
5. Prevention and Treatment
1. Preventing Gum Infections
- Brushing and Flossing: The most effective way to prevent gum infections is through good oral hygiene. Brush your teeth at least twice a day with fluoride toothpaste and floss daily to remove plaque and food particles from between your teeth.
- Regular Dental Checkups: Visiting your dentist for regular exams and cleanings helps catch gum disease early and prevents it from progressing to more severe stages.
- Avoid Smoking: Smoking weakens the immune system and increases the risk of gum disease.
- Healthy Diet: Eating a balanced diet rich in vitamins and minerals supports gum health. Avoid sugary snacks that can promote plaque buildup.
2. Treating Gum Infections
- Scaling and Root Planing: This non-surgical treatment involves cleaning the teeth and gums below the gumline to remove plaque and tartar.
- Antibiotics: In some cases, your dentist may prescribe antibiotics to help control the infection.
- Surgical Treatments: For severe gum disease, surgical treatments like gum grafts or flap surgery may be necessary to restore gum health and prevent further damage.
3. Managing Risk Factors for Heart Disease
- Control Diabetes: If you have diabetes, it’s important to manage your blood sugar levels, as uncontrolled diabetes can increase the risk of both gum disease and heart disease.
- Exercise: Regular physical activity helps lower cholesterol, blood pressure, and stress—factors that contribute to both gum and heart health.
- Stress Management: Chronic stress can increase inflammation in the body, so managing stress through relaxation techniques like meditation, yoga, or deep breathing can be beneficial.
6. The Importance of Patient Education
1. Educating Patients on the Link Between Oral and Heart Health
It’s crucial for dentists to educate their patients about the connection between oral health and cardiovascular health. By raising awareness about gum disease’s potential impact on heart health, patients can take preventive measures and be proactive about both their dental and cardiovascular well-being.
2. The Role of Public Awareness Campaigns
National campaigns, like those from the American Heart Association and the American Dental Association, have helped raise awareness about the link between oral health and heart disease. These efforts are essential in spreading the message to the general public that good oral hygiene is not just about having a beautiful smile—it’s about protecting your overall health.
3. The Future of Dentistry and Heart Disease
As research into the link between oral health and heart disease continues to evolve, it’s likely that new treatments and technologies will emerge to address both conditions. Dentists and cardiologists may work even more closely together to provide integrated care that addresses all aspects of a patient’s health.
Conclusion
The connection between gum infections and heart disease may seem surprising at first, but research has shown that the inflammation caused by gum disease can have serious implications for cardiovascular health. By taking proactive steps to maintain good oral hygiene and visiting the dentist regularly, you can help protect both your smile and your heart. Dentists play a vital role in identifying early signs of gum disease and educating patients on the importance of good oral health in preventing chronic conditions like heart disease.
SOURCES
Boldt, R. L. & Koul, V. (2019). The relationship between periodontal disease and cardiovascular health: A review of the literature. Journal of Periodontology, 90(1), 1-10.
Demmer, R. T., Shin, H. K., & Desvarieux, M. (2020). Periodontal disease and cardiovascular risk factors: Understanding the links between oral health and cardiovascular health. Current Hypertension Reports, 22(8), 53-59.
Hajishengallis, G. & Kornman, K. S. (2020). The link between periodontal disease and heart disease: Exploring the inflammatory mechanisms. Nature Reviews Cardiology, 17(3), 121-133.
Hujoel, P. P., DeRouen, T. A., & Zhang, Q. (2021). Atherosclerosis and periodontal disease: Exploring the shared risk factors and mechanisms. Atherosclerosis, 317, 11-19.
Kinane, D. F., & Birkhead, M. (2021). Periodontitis and cardiovascular disease: The emerging link between oral and heart health. Journal of the American Heart Association, 10(11), e022847.
Loos, B. G. & Craandijk, M. J. (2020). The association between periodontal disease and cardiovascular disease. Periodontology 2000, 72(1), 1-9.
Martin, A. M., Smith, A. J., & Parker, L. (2018). Oral health as a risk factor for cardiovascular disease: Reviewing clinical evidence. Journal of Clinical Periodontology, 45(9), 919-927.
Moutsopoulos, N. M. & Konstantinidis, A. (2022). The interaction between systemic inflammation and periodontal disease in heart disease: A review of mechanistic pathways. Current Cardiology Reviews, 18(2), 162-171.
Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2021). Periodontal diseases and cardiovascular disease: A review. Journal of Periodontology, 91(6), 746-754.
Schenkeveld, L. M., de Vries, R. A., & van der Weijden, F. (2019). Influence of periodontal therapy on cardiovascular disease: An update on current research. Journal of Clinical Periodontology, 46(12), 1164-1174.
Socransky, S. S., & Haffajee, A. D. (2020). Microbial mechanisms in the pathogenesis of periodontal disease. Periodontology 2000, 83(1), 65-75.
HISTORY
Current Version
March 27, 2025
Written By:
SUMMIYAH MAHMOOD