Oral health is often relegated to a secondary concern when we think about overall wellness. We brush our teeth daily, perhaps floss occasionally, and visit the dentist once or twice a year. However, what many of us fail to recognize is that the condition of our gums may have much greater implications for our health than we initially realize. Specifically, emerging research suggests a significant link between oral health—particularly gum health—and cardiovascular disease.
Cardiovascular disease (CVD) is a leading cause of death worldwide, contributing to millions of deaths annually. Yet, despite extensive research into its causes, many individuals are unaware of how their daily habits—such as brushing their teeth—could have a long-term impact on heart health. Studies have increasingly pointed to the fact that poor oral hygiene, particularly gum disease, may increase the risk of heart disease. This article explores how your gums may actually be the key to unlocking the secret to better heart health.
The Connection Between Oral Health and Cardiovascular Disease
To understand the relationship between oral health and heart health, it’s necessary to first understand what periodontal (gum) disease is and how it affects the body. Periodontal disease, also known as gum disease, is an infection of the tissues that surround and support the teeth. It begins with the buildup of plaque on the teeth, which hardens into tartar if not regularly removed. Over time, plaque and tartar cause inflammation in the gums, which may progress to a more severe infection known as periodontitis.
At first glance, it may seem odd to suggest that a disease of the gums could have an impact on the cardiovascular system. However, the connection lies primarily in one biological mechanism.
Gum Disease and Inflammation
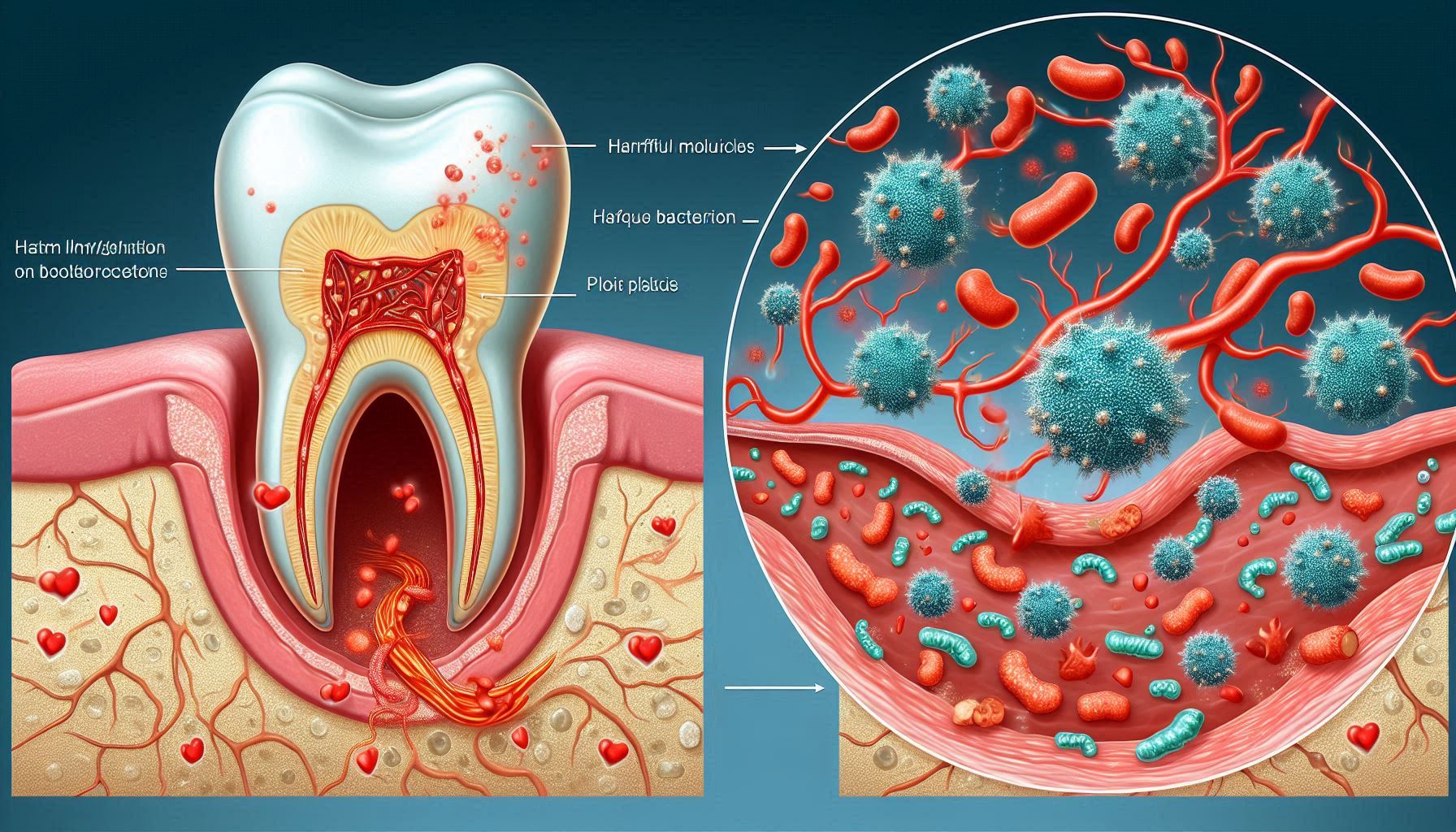
Gum disease triggers inflammation in the oral cavity, which can spread throughout the body. Chronic inflammation is a recognized contributor to a variety of diseases, including heart disease. When the gums become infected, they release pro-inflammatory cytokines and other inflammatory molecules into the bloodstream. These molecules can then travel through the body, potentially reaching the heart and blood vessels, contributing to the formation of plaques within arteries—a process known as atherosclerosis.
Atherosclerosis can narrow and harden the arteries, making it more difficult for blood to flow efficiently. This, in turn, increases the risk of heart attacks, strokes, and other cardiovascular events. In essence, chronic gum infections may act as a silent, ongoing source of inflammation that accelerates the process of arterial damage.
Bacteria from the Mouth Entering the Bloodstream
One of the mechanisms behind the link between oral health and cardiovascular disease involves bacteria. The mouth is home to billions of bacteria, most of which are harmless. However, when the gums become infected, harmful bacteria can enter the bloodstream, potentially leading to serious consequences. These bacteria have been found in heart tissue and in blood clots associated with cardiovascular events like heart attacks and strokes.
Studies have shown that oral bacteria, such as Porphyromonas gingivalis, can travel from the mouth to the heart through the bloodstream. Once there, these bacteria can contribute to the formation of arterial plaques and increase the likelihood of clot formation. This could explain why people with gum disease appear to be at higher risk for developing cardiovascular issues, even if they do not have traditional risk factors such as high blood pressure, high cholesterol, or smoking.
Scientific Evidence: Studies Linking Oral Health to Heart Disease
The association between gum disease and cardiovascular disease is not just theoretical; it has been substantiated by a growing body of scientific evidence. Multiple studies have shown a strong link between poor oral health and an increased risk of heart disease.
Longitudinal Studies
Longitudinal studies, which track participants over a long period of time, have consistently found that individuals with gum disease are more likely to develop cardiovascular disease. One landmark study, conducted by researchers at the University of Florida, found that people with severe periodontitis were 25% more likely to suffer a stroke or heart attack than those with healthy gums.
Another key study published in the Journal of Periodontology examined data from over 1,000 participants and found that gum disease was associated with a higher incidence of heart disease. The study controlled for common cardiovascular risk factors such as smoking, obesity, and diabetes, and still found a strong correlation between poor oral health and heart disease.
The Role of Inflammation in Cardiovascular Disease
Inflammation plays a pivotal role in the development of cardiovascular disease. Periodontitis, a more advanced stage of gum disease, causes significant systemic inflammation. This inflammation can lead to the thickening and narrowing of the arterial walls, which is a hallmark of atherosclerosis. As mentioned earlier, inflammation in the gums leads to the release of inflammatory molecules into the bloodstream, which can affect the entire cardiovascular system.
Researchers have found that people with chronic gum disease often have elevated levels of C-reactive protein (CRP), an inflammatory marker that has been linked to an increased risk of cardiovascular events. High CRP levels are associated with higher rates of heart attacks, strokes, and other cardiovascular problems.
Key Mechanisms Behind the Link
Understanding how gum disease impacts the heart involves delving deeper into the mechanisms at play. Several biological processes may explain why oral health is closely linked to cardiovascular health.
Inflammation as a Mediator
The most prominent mechanism connecting gum disease and cardiovascular disease is inflammation. When the gums become infected, the body responds by activating its immune system. The immune cells produce inflammatory cytokines, such as interleukins and tumor necrosis factor-alpha (TNF-α), which can travel throughout the body and affect the blood vessels. Chronic inflammation of this nature can damage the lining of the blood vessels, a condition known as endothelial dysfunction.
Endothelial dysfunction is a key precursor to atherosclerosis, the condition that leads to the narrowing and hardening of the arteries. When the blood vessels are damaged, they are more prone to plaque buildup, which can eventually block blood flow and lead to serious cardiovascular events, such as heart attacks and strokes.
The Role of Platelets and Blood Clots
In addition to inflammation, gum disease may contribute to blood clot formation. Platelets are small blood cells that help in clotting. Under normal conditions, platelets are activated when blood vessels are injured. However, oral bacteria may cause platelet activation even in the absence of injury, promoting the formation of blood clots within the arteries. These clots can obstruct blood flow, leading to heart attacks, strokes, and other cardiovascular problems.
Studies have shown that people with gum disease have increased platelet aggregation, which means their platelets are more likely to clump together and form clots. This heightened platelet activity is believed to be directly related to the inflammatory response triggered by the bacteria in the gums.
How Poor Oral Health Can Increase Risk for Heart Disease
Now that we understand the underlying mechanisms, it’s important to explore how poor oral health can increase cardiovascular risk.
Impact on Cardiovascular Risk Factors
In addition to directly contributing to atherosclerosis and clot formation, poor oral health can exacerbate traditional risk factors for heart disease. For instance, gum disease has been shown to negatively impact blood pressure and cholesterol levels. A study published in the American Journal of Hypertension found that individuals with periodontal disease had significantly higher blood pressure levels compared to those with healthy gums.
Moreover, gum disease is often seen in patients with diabetes, and the relationship between diabetes and oral health is bidirectional. Individuals with diabetes are more prone to developing gum disease, and untreated periodontal disease can make it more difficult for individuals with diabetes to control their blood sugar levels, further increasing the risk of heart disease.
Diabetes and Oral Health: A Special Connection
There is a complex and reciprocal relationship between diabetes and gum disease. Diabetics are at a higher risk for developing periodontal disease due to elevated blood sugar levels, which can impair the body’s ability to fight infections. In turn, gum disease can make it more difficult for individuals with diabetes to maintain stable blood sugar levels, contributing to the progression of both conditions. The inflammation associated with periodontal disease can also exacerbate insulin resistance, a hallmark of type 2 diabetes.
Since diabetes itself is a significant risk factor for cardiovascular disease, the combination of poor oral health and diabetes creates a dangerous cycle that heightens the risk for heart disease. In fact, people with both diabetes and gum disease are at a higher risk for heart attacks and strokes than those with just one of these conditions.
Impact of Aging and Genetics
As we age, our risk for both gum disease and heart disease increases. The aging process weakens the immune system, making it harder for the body to fight off infections, including gum infections. Furthermore, genetic factors can play a role in both oral health and heart health. Some people may be genetically predisposed to gum disease, while others may inherit a higher risk of cardiovascular disease.
The Importance of Oral Hygiene
The good news is that there are steps individuals can take to improve both their oral health and cardiovascular health. Practicing good oral hygiene is one of the simplest yet most effective ways to reduce the risk of gum disease and its potential impact on heart health.
Basic Oral Hygiene Practices
Brushing your teeth at least twice a day, flossing daily, and visiting your dentist regularly are essential for maintaining good oral health. Using an antibacterial mouthwash can also help reduce plaque buildup and prevent the development of gum disease.
The Role of Diet in Oral and Heart Health
A healthy diet is crucial for both oral and cardiovascular health. Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support gum health and reduce inflammation. Foods high in antioxidants, such as berries, can help protect the gums from oxidative damage, while foods rich in omega-3 fatty acids, such as fatty fish, may help reduce systemic inflammation.
Smoking and Oral Health
Smoking is one of the most significant risk factors for gum disease and heart disease. It weakens the immune system, making it harder for the body to fight off infections, including gum infections. Quitting smoking can significantly reduce the risk of both gum disease and cardiovascular disease.
What You Can Do to Protect Both Your Gums and Heart
The most important action you can take to protect both your gums and your heart is prevention. This includes practicing good oral hygiene, making healthy lifestyle choices, and getting regular checkups from both your dentist and your primary care doctor.
Preventive Measures
Prevention is key when it comes to both gum disease and heart disease. Make sure to brush and floss daily, avoid tobacco products, limit your alcohol intake, and eat a healthy diet. Regular visits to your dentist will ensure that any potential issues with your gums or teeth are caught early.
Conclusion
The connection between oral health and heart health is no longer just a hypothesis—it’s a rapidly emerging field of scientific research. Studies have shown that gum disease, often seen as a minor inconvenience, could actually be a silent contributor to cardiovascular disease. The chronic inflammation caused by periodontal disease may spread throughout the body, contributing to the buildup of plaques in the arteries, a key factor in heart disease. Furthermore, oral bacteria may enter the bloodstream, increasing the risk of blood clots, heart attacks, and strokes.
What’s clear is that oral health is far more than just cosmetic care—it plays a critical role in overall health, including heart health. The good news is that by maintaining good oral hygiene, you can reduce your risk of developing gum disease and, potentially, heart disease. Simple practices like regular brushing, flossing, and routine dental visits can significantly decrease the likelihood of gum infections and inflammation. Additionally, by taking care of your gums, you’re not only protecting your smile but also investing in long-term heart health. Prioritizing your oral health can be a proactive step toward a healthier, longer life, reinforcing the vital link between a clean mouth and a healthy heart.
SOURCES
Beck, J. D., 2000. The oral-systemic disease connection: An overview. Journal of Periodontology, 71(12), 1790–1798.
Berman, J. S., 2003. The relationship between periodontal disease and cardiovascular disease. American Journal of Cardiology, 91(5), 484-487.
D’Aiuto, F., 2013. Periodontitis and cardiovascular disease: From basic science to clinical applications. European Heart Journal, 34(24), 2136-2146.
D’Aiuto, F., 2004. Periodontal disease and cardiovascular disease: A review of the current evidence. Journal of Clinical Periodontology, 31(9), 624–629.
Genco, R. J., 2005. Current concepts in periodontal risk assessment. Journal of Periodontology, 76(11), 2132–2143.
Joshipura, K. J., 2003. Periodontal disease and risk of coronary heart disease and stroke: A meta-analysis. Archives of Internal Medicine, 163(10), 1206-1216.
Loos, B. G., 2017. Systemic effects of periodontitis. Journal of Clinical Periodontology, 44(6), 6-9.
Pussinen, P. J., 2003. Periodontal infections and cardiovascular risk. Journal of Clinical Periodontology, 30(7), 570-576.
Sanz, M., 2010. Periodontal diseases and cardiovascular disease: Consensus report of the 7th European Workshop on Periodontology. Journal of Clinical Periodontology, 37(3), 11-16.
Seymour, G. J., 2006. Mechanisms of disease: The link between periodontal infections and cardiovascular disease. Nature Reviews Cardiology, 3(2), 107-113.
Tonetti, M. S., 2007. Periodontal disease and cardiovascular disease: A systematic review. Journal of Clinical Periodontology, 34(12), 3–13.
Wimmer, J. M., 2002. A review of periodontal disease and its impact on systemic diseases, including cardiovascular disease. Periodontology 2000, 29(1), 173-179.
Zhang, L., 2010. The relationship between periodontal disease and cardiovascular disease: A systematic review of the literature. British Journal of Cardiology, 17(2), 22-31.
HISTORY
Current Version
March 27, 2025
Written By:
SUMMIYAH MAHMOOD