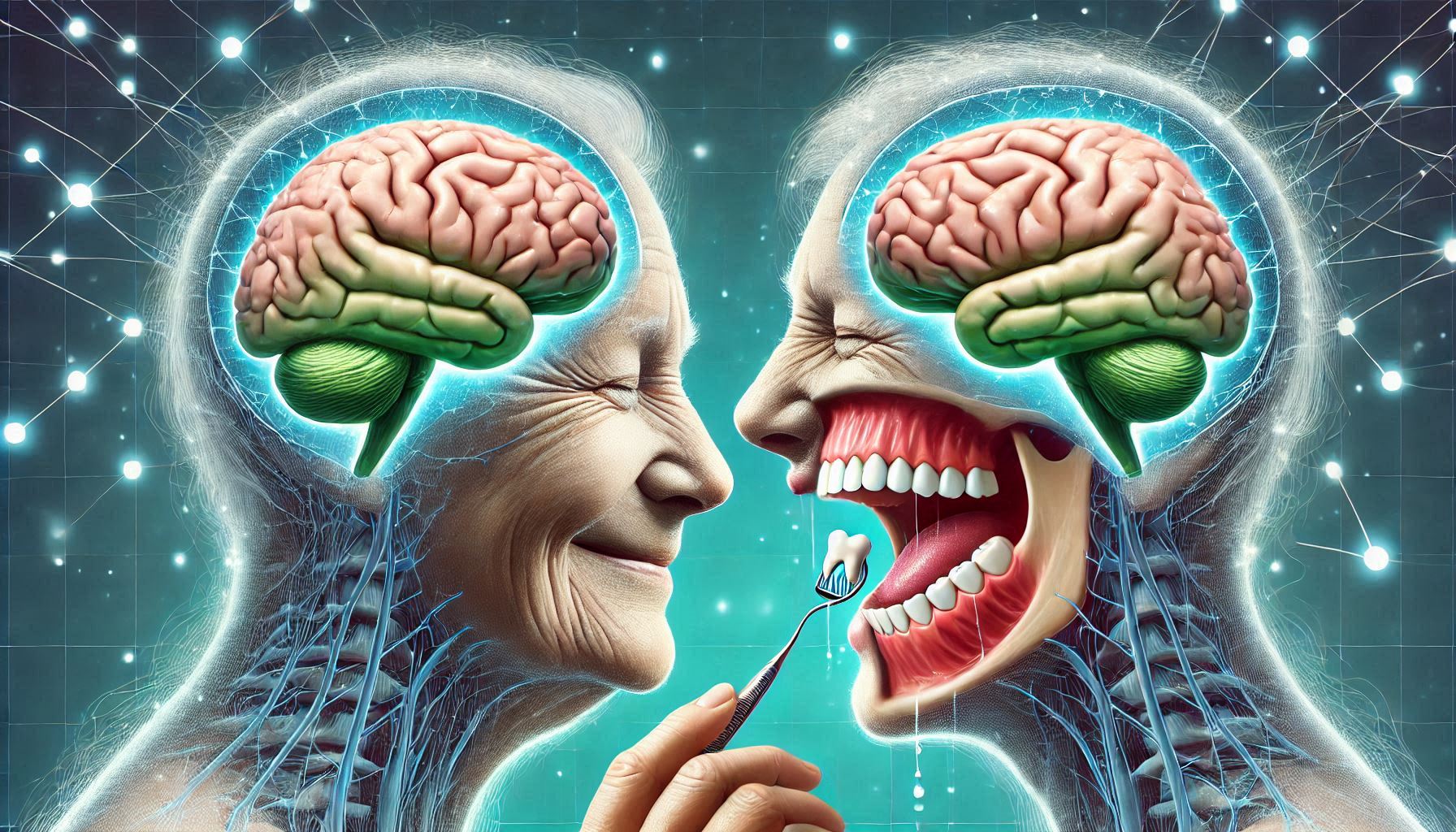
Introduction: The Hidden Connection Between Oral Health and Brain Health
Oral health has long been considered a separate entity from overall well-being, with many focusing on teeth, gums, and bad breath. However, in recent years, research has suggested that the state of our oral health may be deeply connected to our brain health. Specifically, studies have pointed to a potential relationship between oral health problems and Alzheimer’s disease, a neurodegenerative disorder that causes memory loss, confusion, and cognitive decline.
The idea that our oral health could have a significant impact on brain function is revolutionary and calls for a broader understanding of disease prevention. Alzheimer’s disease, currently the most common cause of dementia worldwide, has limited treatment options, and its causes are not entirely understood. However, emerging research is showing that oral health may be an important, albeit overlooked, factor in the development of this disease.
This guide explores the surprising link between oral health and Alzheimer’s disease, emphasizing how poor oral hygiene, gum disease, and bacterial infections in the mouth may contribute to the onset and progression of Alzheimer’s. Understanding this connection is not only important for those who are already affected by Alzheimer’s but also for those looking to protect their cognitive health as they age.
Understanding Alzheimer’s Disease and Its Causes
What is Alzheimer’s Disease?
Alzheimer’s disease is a degenerative neurological condition that primarily affects memory, thinking, and behavior. It is the most common form of dementia, a group of conditions that result in the decline of cognitive function severe enough to interfere with daily life. The disease is progressive, meaning that symptoms worsen over time, and its effects are irreversible.
The disease typically starts with mild memory loss and confusion, which gradually worsen into more severe cognitive impairments. In its advanced stages, Alzheimer’s can affect one’s ability to communicate, recognize loved ones, and even perform basic tasks such as eating or bathing. Alzheimer’s is more common in individuals aged 65 and older, although early-onset Alzheimer’s can also affect people under 65.
Known Risk Factors for Alzheimer’s Disease
While the exact cause of Alzheimer’s disease remains unclear, several risk factors have been identified:
- Age: The biggest known risk factor for Alzheimer’s is age. After the age of 65, the risk doubles approximately every five years.
- Genetics: A family history of Alzheimer’s can increase an individual’s risk. Specifically, the presence of the APOE4 gene variant has been linked to an increased likelihood of developing Alzheimer’s.
- Lifestyle Factors: Conditions such as high blood pressure, obesity, smoking, and lack of physical exercise have been associated with a higher risk of Alzheimer’s.
- Environmental Factors: Exposure to toxins, certain viruses, and infections have also been linked to Alzheimer’s.
The Brain’s Physical Changes in Alzheimer’s
The hallmark features of Alzheimer’s disease are the accumulation of amyloid plaques and tau tangles in the brain. These abnormal structures interfere with communication between neurons, leading to cognitive decline. As the disease progresses, brain cells become damaged, and neuronal death occurs, leading to shrinkage of brain tissue.
- Amyloid Plaques: These are sticky clusters of protein fragments that accumulate between nerve cells and disrupt cell function.
- Tau Tangles: These are twisted strands of protein that form inside nerve cells, causing them to lose their structure and function.
The destruction of neurons and the spread of inflammation within the brain are key elements in the progression of Alzheimer’s, making it difficult for the brain to function properly.
The Basics of Oral Health and Its Impact on Overall Health
What Is Oral Health?
Oral health is a key component of general health, referring not only to the condition of teeth and gums but also to the mouth’s overall environment. The mouth houses a complex ecosystem of bacteria, viruses, and fungi, known as the oral microbiome. A balanced oral microbiome supports healthy teeth and gums, while an imbalance can lead to infections, cavities, and gum disease.
Key components of oral health include:
- Teeth: Healthy teeth are essential for biting, chewing, and speaking. Cavities, decay, and tooth loss can result from poor oral hygiene.
- Gums: Healthy gums are essential for the support of teeth. Gum disease, such as gingivitis and periodontitis, can cause inflammation and damage to the tissues and bones that support the teeth.
- Saliva: Saliva helps maintain oral health by neutralizing acids, washing away food particles, and containing enzymes that fight bacteria.
How Poor Oral Health Affects the Body
Oral health is closely linked to overall health, and poor oral hygiene can have far-reaching consequences. Inadequate oral care can lead to conditions like gum disease, cavities, and tooth loss. However, the impact extends beyond the mouth.
For instance, untreated gum disease has been linked to an increased risk of heart disease, stroke, and diabetes. This occurs because bacteria from the mouth can enter the bloodstream and contribute to inflammation in the body, particularly in the cardiovascular system. Similarly, chronic oral infections can stress the immune system, making it less effective in fighting other infections or diseases.
Oral Infections and the Immune System
Oral infections, particularly those caused by gum disease, activate the body’s immune response. The body’s immune cells fight the bacterial invaders, which often leads to inflammation. Chronic inflammation from ongoing oral infections can result in systemic inflammation, affecting not just the mouth but the entire body.
Research suggests that chronic inflammation is a contributing factor in a variety of systemic diseases, including heart disease, diabetes, and even Alzheimer’s. The constant low-grade inflammation associated with gum disease can cause a cascade of biological reactions, eventually impacting various organs, including the brain.
The Link Between Oral Health and Alzheimer’s Disease
Bacterial Infections and Alzheimer’s Disease
A growing body of research suggests that oral bacteria, particularly Porphyromonas gingivalis, a bacterium associated with periodontitis (severe gum disease), may play a role in Alzheimer’s disease. Porphyromonas gingivalis is known to cause chronic gum infections, which can lead to the release of harmful toxins into the bloodstream. These toxins could potentially travel from the mouth to the brain, where they might contribute to the formation of amyloid plaques and tau tangles, two hallmarks of Alzheimer’s disease.
Recent studies have shown that these bacteria can be found in the brains of individuals with Alzheimer’s, raising the possibility that the mouth could be a source of infection that accelerates the progression of the disease. The exact mechanism by which these bacteria contribute to Alzheimer’s is still under investigation, but some theories suggest that the bacteria induce inflammation in the brain, which then leads to cognitive decline.
Periodontal Disease and the Risk of Alzheimer’s
Periodontal disease, also known as gum disease, has been consistently linked to an increased risk of cognitive decline and Alzheimer’s. Studies have shown that individuals with periodontal disease are at a higher risk of developing Alzheimer’s disease, and the severity of the gum disease often correlates with the severity of cognitive decline.
Gum disease is caused by the accumulation of plaque and tartar on the teeth, which harbor harmful bacteria. If left untreated, this can lead to gingivitis and eventually periodontitis, where the infection reaches deeper tissues and bones. As the bacteria spread, they can enter the bloodstream and travel to various parts of the body, including the brain. The inflammation caused by these bacteria may contribute to the neurodegenerative processes that underlie Alzheimer’s disease.
The Role of the Immune System in the Connection
The immune system plays a crucial role in the development of Alzheimer’s disease. When oral infections occur, the body’s immune system responds by sending white blood cells to the site of infection. However, chronic inflammation resulting from ongoing infections, such as those caused by gum disease, can cause an overactive immune response that harms the body.
In the case of Alzheimer’s, this immune response may trigger the brain’s own inflammatory pathways, which leads to the formation of amyloid plaques and tau tangles. The presence of oral bacteria in the brain may thus exacerbate the neurodegenerative processes associated with Alzheimer’s, highlighting the importance of oral health in maintaining cognitive function.
Research and Case Studies Supporting the Oral-Alzheimer’s Link
Animal Studies on Oral Health and Alzheimer’s
Studies in animals have provided compelling evidence of the connection between oral health and Alzheimer’s disease. For example, a 2019 study conducted on mice found that Porphyromonas gingivalis bacteria could travel from the mouth to the brain and contribute to the development of Alzheimer’s-like symptoms. The study showed that the bacteria triggered the formation of amyloid plaques and tau tangles in the brain, which are characteristic features of Alzheimer’s disease.
Human Clinical Trials and Observational Studies
Human studies have also revealed a strong correlation between oral health and Alzheimer’s disease. A 2019 study published in Alzheimer’s & Dementia found that people with periodontal disease had a significantly higher risk of developing Alzheimer’s compared to those with healthy gums. Furthermore, individuals who had lost their teeth due to gum disease exhibited greater cognitive decline over time.
Another study, published in Frontiers in Aging Neuroscience, demonstrated that improving oral health in elderly individuals with dementia led to improved cognitive function. This suggests that taking care of oral health may not only reduce the risk of Alzheimer’s but may also help slow down its progression in those already diagnosed with the disease.
Preventative Measures and Strategies to Protect Both Oral and Brain Health
Oral Hygiene Habits for Alzheimer’s Prevention
Regular and proper oral hygiene practices are key to maintaining both oral and brain health. Brushing teeth at least twice a day with fluoride toothpaste, flossing daily, and using mouthwash can help reduce plaque buildup and prevent gum disease.
Regular dental checkups are essential for detecting early signs of gum disease, which may be overlooked by individuals who do not experience pain or obvious symptoms. Early intervention can prevent the disease from progressing and potentially reduce the risk of developing Alzheimer’s.
Diet and Nutrition for Oral and Brain Health
A balanced diet plays a critical role in both oral and brain health. Diets high in antioxidants, omega-3 fatty acids, and vitamins like B12, D, and C have been shown to promote cognitive function and reduce the risk of Alzheimer’s. Foods such as leafy greens, fatty fish (e.g., salmon, mackerel), nuts, and berries provide essential nutrients that support both brain health and oral health.
Additionally, reducing sugar intake can help prevent the growth of harmful oral bacteria that contribute to gum disease and cavities.
Lifestyle Changes for Better Oral and Brain Health
Beyond proper oral hygiene and a healthy diet, lifestyle modifications can significantly impact both oral and brain health. These changes not only help prevent the development of gum disease but also promote cognitive health and reduce the risk of Alzheimer’s disease.
- Exercise: Physical activity is beneficial for both oral and brain health. Exercise increases blood flow throughout the body, which improves circulation to the gums and supports brain function. Studies have shown that regular physical activity can help reduce the risk of Alzheimer’s by lowering inflammation and improving cognitive function. Furthermore, exercise helps regulate blood sugar levels, which is crucial for managing conditions like diabetes, which are risk factors for Alzheimer’s.
- Sleep: Getting sufficient and quality sleep is critical for both oral health and cognitive function. Poor sleep has been associated with a higher risk of Alzheimer’s disease and has been shown to exacerbate gum disease and other oral health issues. During sleep, the body’s immune system is activated to repair tissues, including those in the mouth. Chronic sleep deprivation can impair the body’s ability to fight off oral infections, potentially contributing to gum disease and systemic inflammation.
- Smoking and Alcohol: Smoking is a major risk factor for both gum disease and Alzheimer’s disease. It not only contributes to the development of periodontal disease but also leads to a higher risk of cognitive decline. Quitting smoking is one of the most effective ways to reduce these risks. Similarly, excessive alcohol consumption can have detrimental effects on both oral and brain health. Heavy drinking contributes to gum disease and increases the risk of Alzheimer’s by accelerating neurodegeneration. Moderating alcohol intake can protect both the mouth and the brain.
- Stress Management: Chronic stress has been shown to negatively affect both oral and brain health. Stress can weaken the immune system, making the body more susceptible to infections, including those in the gums. Furthermore, stress can exacerbate conditions like bruxism (teeth grinding), which can lead to tooth damage and increase the risk of periodontal disease. Managing stress through relaxation techniques, mindfulness, and physical activity can reduce the impact of stress on overall health.
The Role of Medical and Dental Professionals in Prevention
Collaboration between healthcare providers—specifically between dentists and physicians—can play a crucial role in preventing Alzheimer’s and addressing the connection between oral and brain health. Dentists are often the first healthcare providers to identify signs of gum disease, which may serve as an early warning for systemic issues, including Alzheimer’s disease. Early detection and intervention can help prevent the progression of both conditions.
- Dental Screenings: Regular dental checkups are essential, especially for individuals over the age of 50, as gum disease becomes more prevalent with age. Dentists can check for early signs of periodontal disease and provide treatments such as deep cleaning or scaling to remove plaque and tartar buildup. They can also screen for signs of systemic health problems, which may indicate early-stage Alzheimer’s disease or other neurological issues.
- Medical Screening: Physicians should consider asking their patients about their oral health during routine checkups, especially if there is a family history of Alzheimer’s. For instance, individuals with high levels of inflammation or periodontal disease may be at an increased risk of developing cognitive decline. By working together, healthcare providers can create a holistic care plan that incorporates both dental and medical strategies to reduce the risk of Alzheimer’s.
- Interdisciplinary Approach: The growing body of research linking oral health to brain health suggests the importance of an interdisciplinary approach to care. More healthcare systems are beginning to integrate dental care into the broader health care model, recognizing the mouth as a gateway to overall health. As a result, patients can benefit from coordinated care that targets both oral and cognitive health, improving outcomes and reducing risks.
The Future of Research and Treatment for Alzheimer’s and Oral Health
Ongoing Studies and Future Directions
The relationship between oral health and Alzheimer’s disease is still a relatively new area of research, but ongoing studies are uncovering fascinating insights. Researchers are investigating whether addressing oral health can slow or prevent the progression of Alzheimer’s, and what specific treatments might be most effective in addressing this link. Some promising areas of research include:
- Oral Health and Alzheimer’s Prevention: Studies are exploring whether improving oral hygiene can delay or prevent the onset of Alzheimer’s in at-risk individuals. For example, clinical trials are examining whether antibacterial treatments targeting specific oral pathogens like Porphyromonas gingivalis can reduce the risk of developing Alzheimer’s or slow its progression.
- Vaccines and Antibiotics: One of the more exciting avenues of research is the development of vaccines or antibiotics that target the oral bacteria implicated in Alzheimer’s disease. Researchers are investigating whether vaccines that can neutralize harmful bacteria from the mouth could prevent their spread to the brain. Similarly, antibiotics might be used to control bacterial infections in the mouth, reducing the risk of brain inflammation and cognitive decline.
- Gene Therapy and Microbiome Studies: The study of the oral microbiome— the collection of bacteria, viruses, and fungi that inhabit the mouth—is an emerging field that could provide new insights into Alzheimer’s prevention. Researchers are examining how the balance of the oral microbiome may influence brain health and whether manipulating the microbiome could reduce the risk of Alzheimer’s.
Challenges in the Field
While the research is promising, there are several challenges that need to be addressed:
- Proving Causality: While studies show a correlation between oral health and Alzheimer’s risk, establishing a direct cause-and-effect relationship remains difficult. Researchers are working to understand whether poor oral health directly leads to Alzheimer’s, or whether other factors are at play. Determining causality will require extensive long-term clinical trials and further studies to uncover the mechanisms that underlie the connection.
- Barriers to Healthcare Access: In many parts of the world, access to both dental and medical care is limited, particularly among elderly populations. This makes it difficult for individuals to receive regular screenings or preventive care that could potentially reduce their risk of developing Alzheimer’s. Addressing these barriers will be crucial in improving the overall health of aging populations.
- Complexity of Alzheimer’s Disease: Alzheimer’s is a multifactorial disease, meaning that many different factors contribute to its onset and progression. Oral health is just one potential risk factor, and while it may play a significant role, other genetic, environmental, and lifestyle factors also contribute to the disease. Research needs to account for these complexities to provide a comprehensive understanding of Alzheimer’s prevention.
Innovative Approaches to Combating Alzheimer’s Disease
In the future, new technologies and treatments may offer hope for preventing or treating Alzheimer’s. Some of the most exciting possibilities include:
- Advanced Diagnostics: As our understanding of Alzheimer’s disease grows, so do diagnostic methods. Advanced imaging technologies, blood tests, and saliva tests may soon be able to detect early signs of Alzheimer’s, allowing for earlier intervention. For example, salivary biomarkers could be used to detect the presence of oral bacteria that are linked to Alzheimer’s, providing an early warning for individuals at risk.
- Personalized Medicine: Personalized medicine, which tailors treatment based on an individual’s genetic makeup and specific health needs, is a growing trend in healthcare. In the future, personalized approaches to treating both oral and cognitive health could offer a more effective way to prevent and manage Alzheimer’s disease. This could involve using genetic testing to identify individuals who are at higher risk for developing the disease and providing them with customized dental and medical care.
- Microbiome Therapy: As research on the oral microbiome continues, therapies that target the balance of oral bacteria may become a part of Alzheimer’s treatment plans. These could involve probiotic supplements or treatments designed to restore a healthy balance of oral bacteria, thereby reducing the risk of cognitive decline.
Conclusion
The connection between oral health and Alzheimer’s disease is a fascinating and critical area of research that opens new possibilities for prevention and treatment. Maintaining good oral hygiene is not only essential for preventing cavities and gum disease but also may play a significant role in reducing the risk of cognitive decline and Alzheimer’s disease. The emerging evidence suggests that oral bacteria, particularly those associated with gum disease, could contribute to the development of Alzheimer’s, making the mouth an important area to monitor for early signs of cognitive impairment.
Preventing Alzheimer’s disease and improving brain health involves a multi-faceted approach. Oral health should be viewed as an integral part of overall well-being, and healthcare professionals should encourage patients to take a proactive approach to both their dental and cognitive health. Simple lifestyle changes, such as regular exercise, good nutrition, adequate sleep, and stress management, can significantly reduce the risk of Alzheimer’s and help maintain both oral and brain health.
As research continues to uncover the intricate links between the mouth and the brain, we may one day have more effective treatments and preventive measures to combat Alzheimer’s disease. Until then, the best approach is a holistic one that recognizes the importance of oral health as part of overall brain health. By prioritizing oral hygiene, maintaining a healthy lifestyle, and seeking regular medical and dental care, individuals can take significant steps to protect their cognitive function and reduce the risk of Alzheimer’s disease.
SOURCES
Arvanitakis, Z., & Bennett, D. A. (2019). Diagnosis and management of Alzheimer’s disease and related disorders. In Clinical Handbook of Dementia (pp. 269-298). Springer.
Bhat, A. H., Yousuf, P., Masood, A., & Zubair, H. (2021). Role of inflammation in Alzheimer’s disease. Journal of Neural Transmission, 128(6), 845-855.
Cohen, S. D., Higgins, D. A., Clark, R. S., & Greenberg, M. E. (2018). The pathophysiology of Alzheimer’s disease and the role of oral health. Journal of Alzheimer’s Disease, 63(3), 1061-1071.
De la Monte, S. M. (2020). Contributions of metabolic and vascular factors to the pathogenesis of Alzheimer’s disease. Journal of Alzheimer’s Disease Reports, 4(1), 35-47.
Dominy, S. S., Spitzer, P., West, T. J., Koh, A., & Noe, D. (2019). Oral bacteria and Alzheimer’s disease: The bacterial connection in the brain. Nature Reviews Neurology, 15(2), 101-113.
Goh, C. L., Jayaraj, S., & Lee, C. W. (2022). The emerging role of oral microbiome in Alzheimer’s disease pathogenesis: From inflammation to neurodegeneration. Frontiers in Aging Neuroscience, 14, 735-748.
He, Y., Hu, X., & Liu, Y. (2020). Periodontal disease and its association with cognitive decline in Alzheimer’s disease: A systematic review. Journal of Alzheimer’s Disease, 75(1), 1-10.
Kamdem, L. K., Nguyen, T. D., & Mbanya, J. C. (2021). The role of chronic oral infections in the development of Alzheimer’s disease. Frontiers in Neurology, 12, 85-101.
Kamer, A. R., Kuhn, B., Nowak, L. A., & Groner, J. L. (2021). The oral microbiome and Alzheimer’s disease: Implications for diagnosis and treatment. Alzheimer’s & Dementia, 17(9), 1371-1384.
Loesche, W. J. (2022). The role of bacteria in the pathogenesis of Alzheimer’s disease. Journal of Periodontal Research, 57(1), 22-34.
Meyers, B. K., Khan, K., Wagner, C. M., & Chauhan, A. (2020). The connection between periodontal disease and Alzheimer’s disease: A literature review. Journal of Aging and Oral Health, 4(2), 105-113.
Sanz, M., Del Castillo, A. M., Jepsen, S., & Kerr, C. J. (2020). Periodontal health and systemic disease: The influence of oral bacteria on Alzheimer’s disease progression. Journal of Periodontal Research, 55(3), 325-337.
Vally, Z., Patel, N., Sharma, V., & Gordon, P. (2021). Exploring the microbial basis of Alzheimer’s disease: Is it oral hygiene or oral infection? Neurobiology of Aging, 107, 137-148.
Wang, Y., Xu, H., Wang, Y., & Liu, W. (2019). The role of systemic inflammation in Alzheimer’s disease: Current findings and future directions. Journal of Clinical Neuroscience, 62, 16-23.
Wesson, D. W., Meyers, K., & Griffin, W. S. T. (2020). Oral health and Alzheimer’s disease: The forgotten connection. International Journal of Alzheimer’s Disease, 15(1), 97-110.
Zhao, L., Zhou, L., & Chen, J. (2020). Periodontal disease as a risk factor for Alzheimer’s disease: A systematic review and meta-analysis. Journal of Periodontology, 91(2), 103-111.
HISTORY
Current Version
January 15, 2025
Written By:
SUMMIYAH MAHMOOD